Edema Treatment for Eyes and Systemic Swelling: Medical Approaches
Fluid buildup in tissues — edema — can affect many parts of the body, including the eye, and treatment depends on the underlying cause. This article summarizes common diagnostic steps and evidence-based medical treatments for different types of edema, explains how swelling can affect vision and overall health, and outlines when to seek care from local services or specialists.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
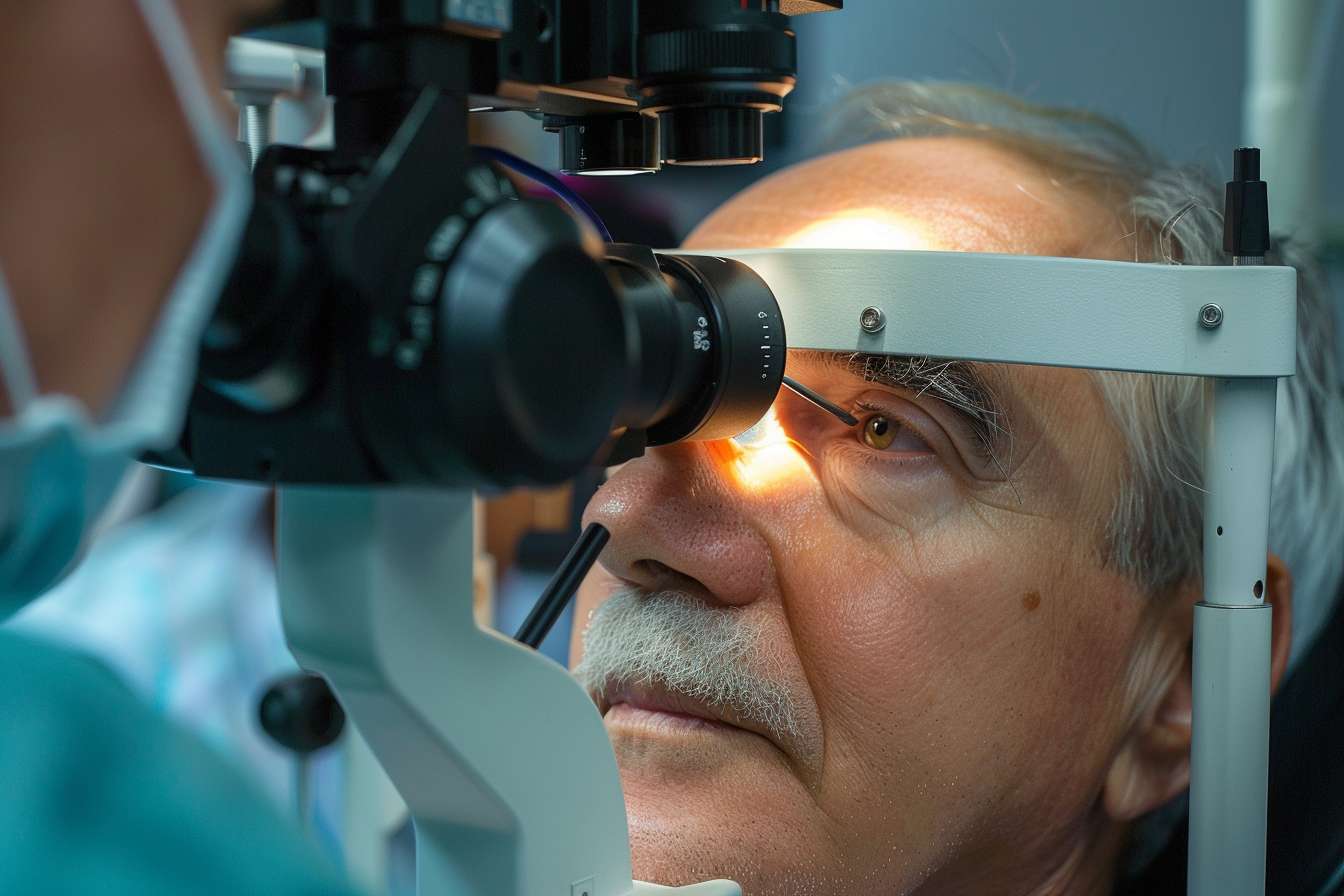
eye: how ocular edema is identified and managed
Ocular edema can involve the eyelids, conjunctiva, cornea, or deeper structures. External swelling (e.g., eyelid edema) often responds to cold compresses, elevation, allergy treatments, or topical medications. Corneal edema may be treated with hyperosmotic drops or ointments to draw out fluid, while severe or chronic corneal swelling sometimes requires surgical options such as endothelial keratoplasty. Diagnosis typically begins with a slit-lamp exam and may include pachymetry or specular microscopy. Treatment targets both symptom relief and the underlying cause, such as allergies, infection, trauma, or endothelial dysfunction.
vision: how swelling affects sight and functional outcomes
Edema that involves ocular structures can blur vision, distort images, and reduce contrast sensitivity. Macular edema — fluid accumulation in the central retina — directly impairs sharp central vision and reading ability. Even transient swelling can affect daily tasks and increase fall risk in older adults. Visual outcomes depend on promptness of treatment, severity, and cause. Regular monitoring with visual acuity checks and optical coherence tomography (OCT) helps clinicians track improvement and adapt therapy to preserve or restore vision.
health: systemic causes and lifestyle-related management
Edema is often a sign of systemic issues such as heart failure, kidney disease, liver disease, venous insufficiency, or lymphedema. General health measures that reduce peripheral edema include sodium reduction in the diet, gradual weight management, leg elevation, and appropriate physical activity. Treating the root medical condition is essential: for example, optimizing heart function can markedly reduce fluid retention. For lymphedema, conservative therapies like manual lymphatic drainage and compression garments are cornerstone measures that support long-term tissue health.
medical: diagnostic tests and commonly used therapies
A clinical exam guides choice of tests: blood work (electrolytes, renal and liver panels), chest X-ray, echocardiography, venous duplex ultrasound, and targeted imaging like OCT for retinal evaluation. Medical therapies include diuretics for volume overload, steroids for inflammatory or allergic edema, and anti-VEGF agents for certain retinal and macular edemas. In some cases, antibiotics or antivirals treat infectious causes. Interdisciplinary care — involving primary care, cardiology, nephrology, dermatology, or ophthalmology — ensures comprehensive evaluation and safer medication management.
retina: treatments for retinal and macular edema
Retinal swelling, particularly macular edema, often requires specialized ophthalmic interventions. First-line treatments may include intravitreal anti-VEGF injections that reduce vascular permeability and fluid accumulation. Corticosteroid injections or implants are alternatives in specific situations, especially if inflammation plays a major role. Laser photocoagulation remains useful for select patterns of retinal vascular leakage. Surgical options such as vitrectomy are reserved for persistent or tractional cases. Monitoring with OCT helps measure response and schedule repeat therapies as needed.
Conclusion
Edema encompasses a wide range of conditions from mild, transient swelling to sight-threatening retinal fluid. Effective treatment starts with accurate diagnosis and addressing the underlying cause, using a mix of lifestyle measures, systemic therapies, and targeted procedures for ocular involvement. Coordination with appropriate medical specialists and regular follow-up are important to monitor response and prevent recurrence. If swelling affects your eye, vision, or overall functioning, seek evaluation by qualified clinicians and consider local services or specialists in your area for tailored care.




