Follow-up Care and Recovery After Floaters Intervention
Follow-up care after an intervention for floaters is critical to monitor healing, identify complications, and support visual recovery. This article outlines typical post-procedure expectations, recommended imaging and consultations, symptom tracking, and practical recovery tips to help patients and clinicians plan effective aftercare.
First few days after a procedure for floaters are often the most sensitive period for vision changes and healing. Patients may notice improved clarity, persistent shadows, or temporary disturbances in vision as the eye adjusts. Regular monitoring during this phase helps clinicians distinguish normal recovery from complications such as increased inflammation, retinal tears, or infection. Understanding expected symptoms, recommended imaging, and the timetable for follow-up visits makes recovery more predictable and improves outcomes for vision and retinal health.
What causes floaters and how do they affect vision?
Floaters are small shapes perceived in the visual field that often originate from changes in the vitreous gel inside the eye. As the vitreous ages or undergoes structural shifts, tiny clumps or strands cast shadows on the retina, creating floaters. While many people adapt to the presence of floaters, they can interfere with tasks that require clear central vision, reading, or detailed work. Distinguishing routine floaters from sudden increases in frequency or flashes of light is essential, since the latter can indicate retinal traction or tears that need urgent ophthalmology assessment.
How is diagnosis and imaging used after intervention?
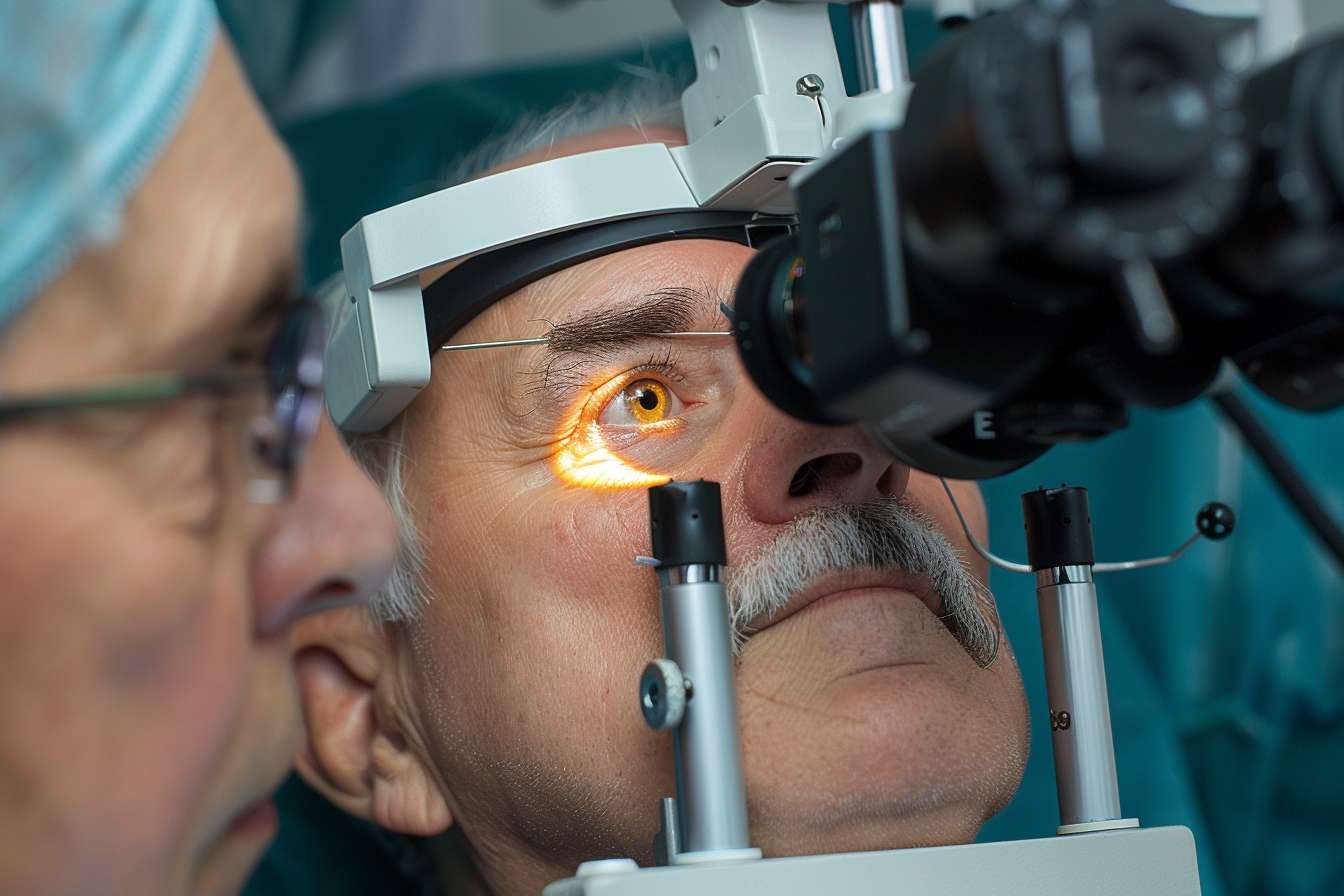
Post-intervention diagnostic steps typically include slit-lamp examination, dilated fundoscopy, and imaging such as optical coherence tomography (OCT) or B-scan ultrasonography when the view to the retina is limited. These modalities allow clinicians to assess the retina’s condition, any residual vitreous debris, and the integrity of retinal layers. Imaging also documents baseline post-procedure anatomy so that subsequent visits can reliably detect changes. Accurate diagnosis and follow-up imaging support decisions about additional treatments or continued observation.
What to expect after laser treatment?
Following laser vitreolysis, patients may see gradual reductions in prominent floaters over weeks to months, though multiple sessions are sometimes required. Immediately after laser treatment, mild discomfort, transient blurring, and a sensation of increased debris are common. Eye pressure and retinal status should be checked within the first week to rule out rare complications. Symptom relief varies: some people report substantial improvement while others notice only modest change; managing expectations through pre-procedure consultation is important.
What to expect after vitrectomy surgery?
Vitrectomy is a surgical option that removes vitreous gel and most visible floaters, typically resulting in significant symptom reduction. Early recovery can include watery eyes, light sensitivity, and temporary blurring as the eye heals and any intraocular gas or tamponade (if used) resolves. Follow-up visits usually occur within 24–72 hours after surgery, then at one week and one month, with additional checks as needed. Monitoring focuses on retinal attachment, intraocular pressure, inflammation, and cataract progression in phakic eyes.
When should I schedule follow-up consultations?
Initial post-procedure follow-up timing depends on the intervention: laser-treated patients commonly return within a week, while surgical cases often require an earlier check within 24–72 hours. Subsequent visits are typically scheduled at one month and three months, with yearly monitoring if recovery is stable. Any sudden increase in floaters, flashes of light, a curtain-like shadow, worsening pain, or rapid vision loss warrants immediate contact with an ophthalmology service, as these may indicate retinal complications that need urgent assessment.
Tips for recovery and long-term eye health
During recovery, adhere to prescribed eye drops and activity recommendations, including temporary restrictions on heavy lifting or strenuous exertion if advised. Wear protective eyewear as recommended and avoid rubbing the eye. Maintain good hydration and manage systemic factors such as blood pressure and diabetes, which can influence retinal health. If imaging is scheduled, attend those appointments to document progress. Communicate new or worsening symptoms promptly to ensure timely evaluation and treatment.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Follow-up care after floaters intervention focuses on monitoring healing, identifying complications early, and supporting visual recovery through appropriate imaging and scheduled consultations. Clear communication between patient and clinician helps set realistic expectations and ensures that any change in symptoms is investigated appropriately. Regular eye assessments and attention to overall eye health support the best possible functional outcomes.




