Glaucoma Treatment: Options, Tests, and Specialist Care
Glaucoma refers to a group of eye conditions that can damage the optic nerve and cause progressive vision loss. Treatments focus on lowering intraocular pressure to slow or prevent further nerve damage. This article describes common approaches, typical tests, and the roles of medical professionals involved in care, helping readers understand what to expect from diagnosis through long-term management.
How does glaucoma affect the eye?
Glaucoma most commonly damages the optic nerve by persistent elevated pressure inside the eye, although some forms occur at normal pressures. The optic nerve carries visual information from the retina to the brain; damage produces gradual peripheral vision loss that can progress to central vision impairment if untreated. Different types—open-angle, angle-closure, normal-tension, and secondary glaucomas—have distinct mechanisms and urgency.
Early disease is often asymptomatic, which is why eye exams that include measuring intraocular pressure and inspecting the optic nerve are important. Regular monitoring can detect structural changes or functional loss on visual field testing before noticeable vision decline.
When should you see an eye doctor?
Anyone with risk factors—age over 60, family history of glaucoma, high myopia, diabetes, African or Hispanic ancestry, a history of eye trauma, or long-term steroid use—should see an eye doctor for screening. Sudden eye pain, nausea, blurred vision, or rainbow halos around lights may indicate an acute angle-closure episode and require urgent evaluation.
Routine comprehensive eye exams typically include pressure checks and optic nerve assessment. If a primary eye doctor (optometrist or general ophthalmologist) identifies suspicious findings, referral to a glaucoma specialist may be recommended for more focused assessment and management.
What medical tests diagnose glaucoma?
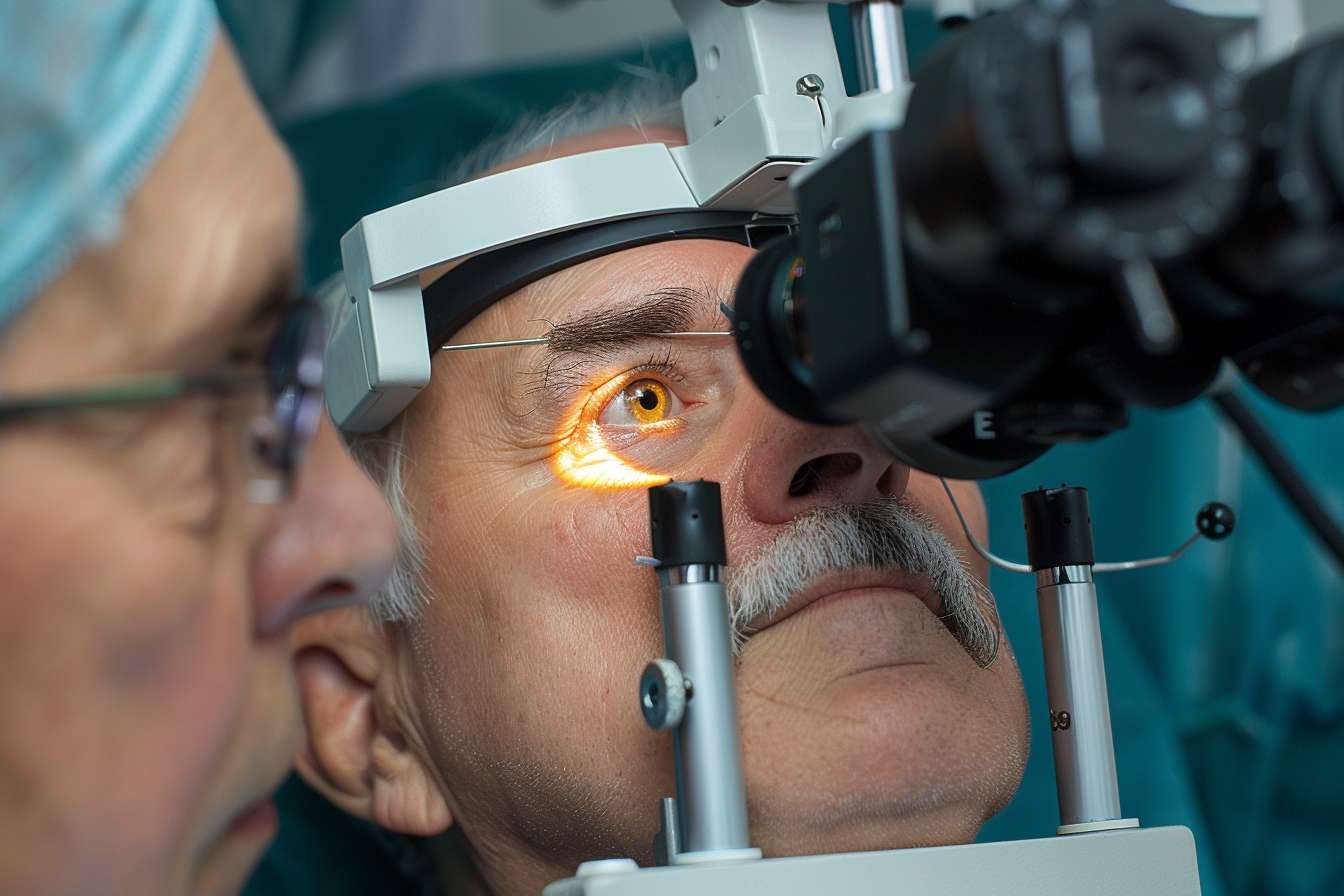
Diagnosis and monitoring rely on a combination of tests. Tonometry measures intraocular pressure. Gonioscopy inspects the drainage angle. Ophthalmoscopy and fundus photography evaluate the optic nerve head. Optical coherence tomography (OCT) provides high-resolution cross-sectional images to detect thinning of the retinal nerve fiber layer. Visual field testing (perimetry) maps functional vision loss.
A single test is rarely definitive; clinicians combine results, trend data over time, and individual risk factors to make a medical diagnosis and decide when to initiate or escalate treatment. Regular testing allows tracking of progression and treatment response.
What care does a glaucoma specialist provide?
A glaucoma specialist is an ophthalmologist with additional training in glaucoma management and surgery. They interpret complex diagnostic data, tailor medical regimens, perform laser procedures such as selective laser trabeculoplasty (SLT), and carry out surgical interventions when necessary. For patients with unstable disease or surgical needs, a specialist can offer options ranging from minimally invasive glaucoma surgeries (MIGS) to more traditional procedures like trabeculectomy or tube shunt implantation.
When seeking local services or referrals in your area, look for a specialist with experience in the specific type of glaucoma diagnosed. A specialist can also coordinate care with primary eye doctors and other medical providers to manage comorbid conditions that affect eye health.
How do glaucoma medications and surgery differ?
Medical therapy typically begins with topical eye drops that lower intraocular pressure by reducing fluid production or improving outflow. Common classes include prostaglandin analogs, beta blockers, alpha agonists, and carbonic anhydrase inhibitors. Side effects can be local (eye redness, irritation) or systemic (rare cardiovascular or respiratory effects), so medical history matters when choosing agents.
Laser treatments such as SLT can lower pressure by improving drainage and are sometimes used as first-line therapy or to reduce medication burden. Surgical options are considered when drops and lasers do not achieve target pressure or when adherence is problematic. Surgeries carry risks such as infection, bleb-related problems, or hypotony (low pressure), but they can provide durable pressure control. Treatment choice is individualized based on disease severity, life expectancy, comorbidities, and patient preferences.
Long-term monitoring and lifestyle considerations
Glaucoma management is usually lifelong. Even after successful treatment, regular visits for pressure checks, OCT scans, and visual field tests are necessary because progression can occur slowly. Adherence to prescribed eye drops is a major factor in treatment success; some patients benefit from reminder systems or caregiver support.
Lifestyle measures—protective eyewear to prevent trauma, smoking cessation, and control of systemic conditions like hypertension and diabetes—support overall eye health. Discuss any supplements, recreational drugs, or over-the-counter medications with your eye doctor, as some agents can affect eye pressure.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Glaucoma treatment involves a combination of accurate testing, individualized medical therapy, and procedural options provided by trained eye care professionals. Early detection and consistent follow-up are central to preserving vision. Treatment plans are tailored to each person’s type of glaucoma, risk profile, and life circumstances, and they may change over time as the disease is monitored.




