Innovations in Neurological Tumor Treatment Protocols
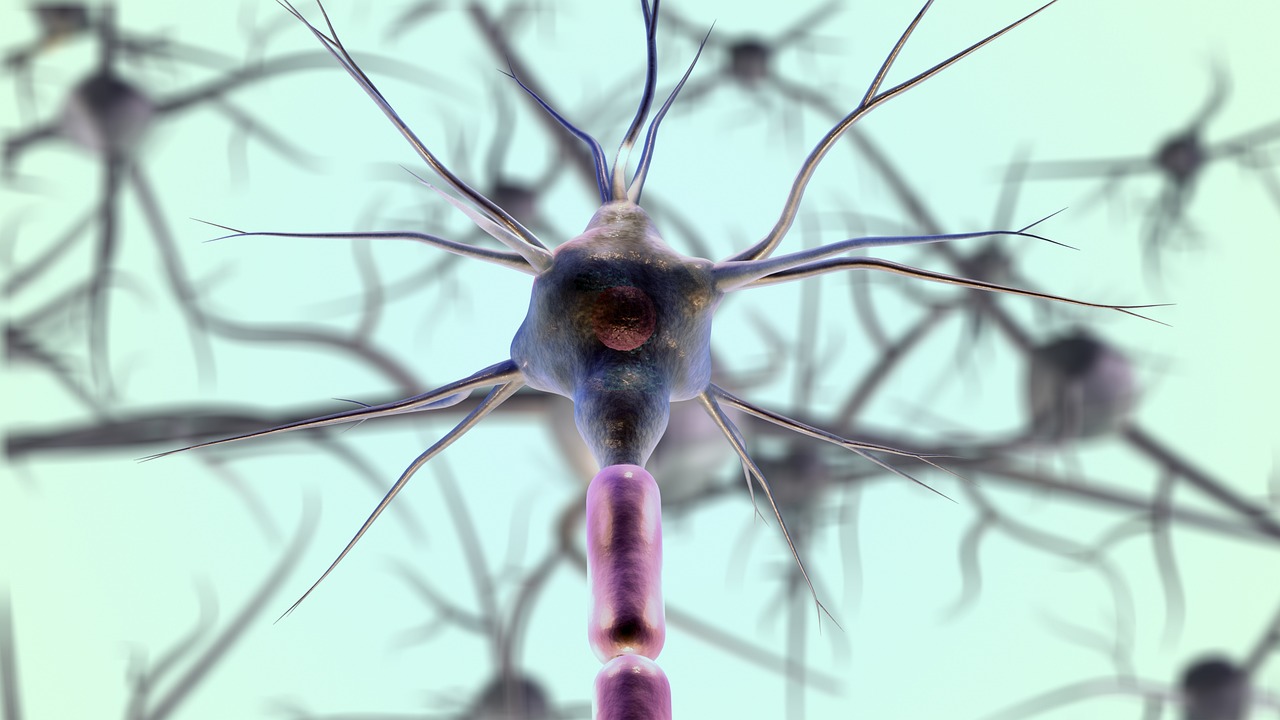
Neurological tumors, often referred to as brain tumors, represent a significant challenge in modern medicine due to their complexity and critical location within the central nervous system. These tumors can originate in the brain (primary) or spread to it from other parts of the body (metastatic), leading to a diverse range of symptoms and treatment approaches. Recent advancements in oncology and neuroscience have brought forth a wave of innovative protocols, enhancing diagnostic precision, therapeutic efficacy, and overall patient care.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Understanding Neurological Tumors: Diagnosis and Pathology
Neurological tumors encompass a broad category of growths that can affect the brain, spinal cord, and surrounding structures. Accurate diagnosis is the cornerstone of effective treatment, relying heavily on advanced imaging techniques and detailed pathology. Magnetic Resonance Imaging (MRI) remains a primary tool for visualizing intracranial and cerebral tumors, providing high-resolution images that help pinpoint tumor location, size, and characteristics. Functional MRI (fMRI) and Diffusion Tensor Imaging (DTI) offer additional insights into brain activity and white matter tracts, crucial for surgical planning.
Pathology plays a vital role in classifying tumors, with biopsies providing tissue samples for microscopic examination. Modern pathology extends beyond traditional histology to include molecular diagnostics, identifying specific genetic mutations and biomarkers. This detailed understanding of a tumor’s molecular profile is increasingly guiding treatment decisions, particularly in the realm of targeted therapies. The integration of advanced imaging and molecular pathology has significantly refined the diagnostic process, leading to more precise and personalized treatment strategies.
Recognizing Symptoms and Promoting Awareness
The symptoms of neurological tumors can vary widely depending on the tumor’s size, type, and location. Common signs may include persistent headaches, seizures, changes in vision, speech difficulties, weakness or numbness on one side of the body, and alterations in personality or cognitive function. These symptoms often develop gradually, making early detection a challenge. Promoting public awareness about these potential indicators is crucial for encouraging timely medical consultation and early diagnosis.
Increased awareness among healthcare providers, especially in primary care settings, can also lead to earlier recognition of subtle neurological changes. Educational campaigns can empower individuals and their families to identify concerning symptoms and seek specialized neurological evaluation promptly. Early identification can significantly impact treatment options and potentially improve outcomes, underscoring the importance of vigilance and informed action.
Advances in Treatment Modalities: Surgery, Radiation, and Chemotherapy
Treatment for neurological tumors often involves a multidisciplinary approach, combining various modalities to achieve the best possible outcome. Surgical resection remains a primary treatment for many tumors, aiming to remove as much of the tumor as safely possible while preserving neurological function. Innovations in neurosurgery include awake craniotomy, intraoperative MRI, and robotic-assisted techniques, enhancing precision and minimizing damage to critical brain areas.
Radiation therapy continues to evolve, with techniques like intensity-modulated radiation therapy (IMRT) and proton therapy offering more precise targeting of tumors while sparing healthy brain tissue. Stereotactic radiosurgery (SRS) delivers highly focused radiation doses in fewer sessions, proving effective for smaller, well-defined tumors. Chemotherapy, often used in conjunction with surgery and radiation, has seen advancements with new drugs and delivery methods, including those designed to cross the blood-brain barrier more effectively. These combined approaches are tailored to the individual patient and tumor characteristics.
Targeted Therapies and Emerging Research in Oncology
The field of oncology has seen remarkable progress with the advent of targeted therapies, which specifically attack cancer cells based on their unique molecular characteristics. For neurological tumors, this includes therapies that inhibit specific growth pathways or angiogenesis (blood vessel formation). Immunotherapy, which harnesses the body’s own immune system to fight cancer, is another promising area of research, with clinical trials exploring its efficacy in various types of brain tumors.
Ongoing research in neuroscience is also investigating novel approaches such as gene therapy, oncolytic viruses, and advanced drug delivery systems. These innovative strategies aim to overcome the challenges posed by the intricate nature of the central nervous system and the aggressive behavior of many neurological tumors. The continuous pursuit of new knowledge and therapeutic avenues offers hope for improved prognosis and quality of life for patients.
Holistic Care and Patient Support
Beyond medical treatments, comprehensive care for individuals with neurological tumors involves extensive support systems. This includes rehabilitation services such as physical, occupational, and speech therapy to address functional deficits resulting from the tumor or its treatment. Psychological support, counseling, and support groups play a crucial role in helping patients and their families cope with the emotional and psychological impact of the diagnosis and treatment journey.
Nutritional guidance and pain management are also integral components of holistic care, focusing on improving overall well-being and managing symptoms. The emphasis on a patient-centered approach ensures that individuals receive not only the most advanced medical interventions but also comprehensive support that addresses their physical, emotional, and social needs throughout their treatment and recovery. This integrated care model is essential for enhancing the quality of life for those affected by neurological tumors.
Continued research and the development of new treatment protocols are transforming the landscape of care for neurological tumors. From advanced diagnostic tools to innovative therapeutic strategies and comprehensive supportive care, the multidisciplinary efforts in neurology and oncology are paving the way for more effective and personalized interventions, ultimately striving to improve patient outcomes and their overall quality of life.




