Personalized Strategies for Pancreatic Well-being
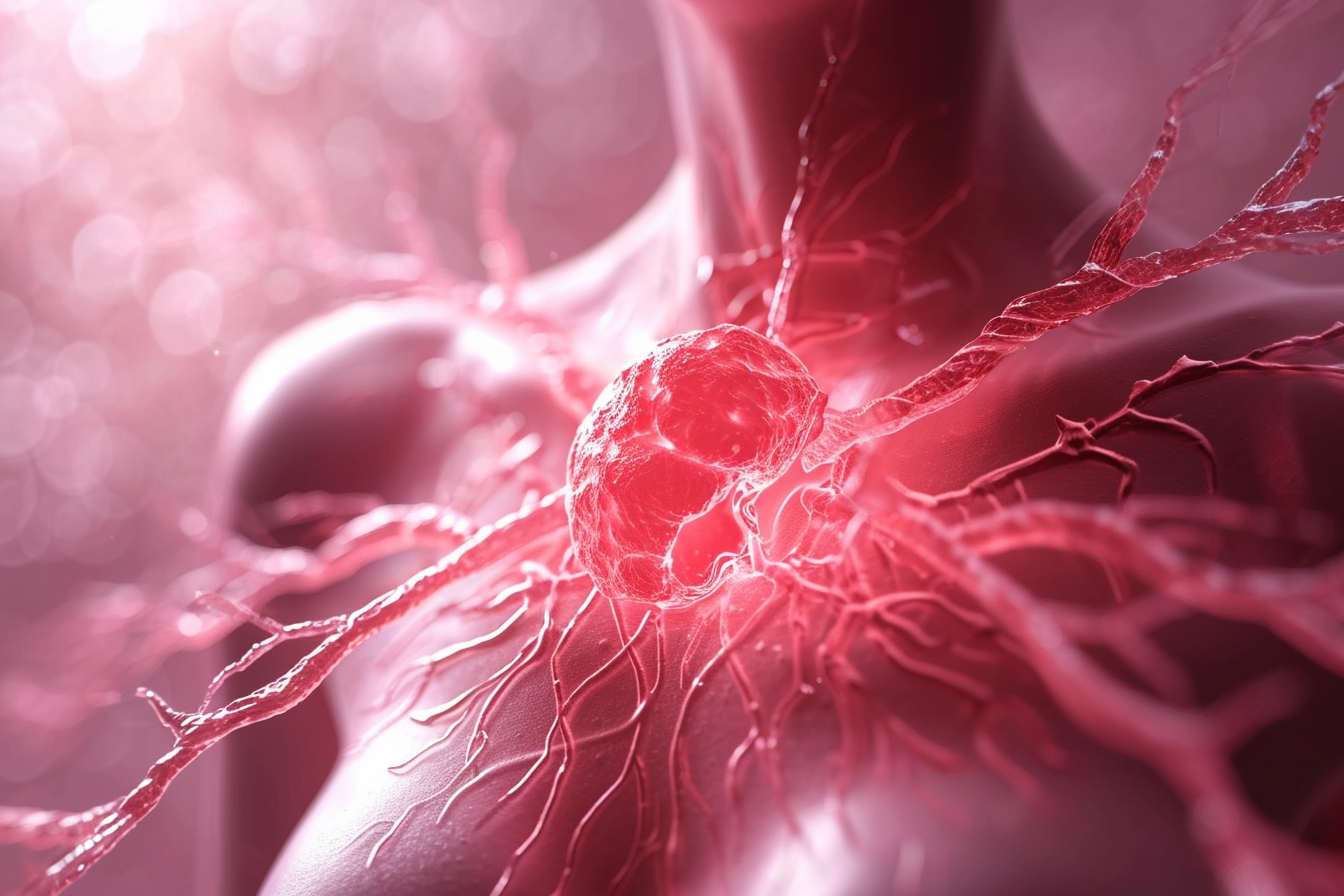
Understanding pancreatic health is crucial for overall well-being, especially when facing complex conditions like pancreatic cancer. Recent advances in medical science and oncology have shifted the focus towards more personalized strategies, recognizing that each patient's journey is unique. These tailored approaches aim to optimize treatment outcomes, enhance quality of life, and provide comprehensive support throughout the disease management process. This article explores various facets of personalized care, from early diagnosis to innovative therapies and long-term wellness planning, emphasizing a holistic view of patient care.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
The pancreas is a vital organ responsible for producing enzymes essential for digestion and hormones like insulin, which regulates blood sugar. When conditions such as pancreatic cancer arise, the complexity of its location and often late diagnosis present significant challenges. However, ongoing research and clinical studies are continuously refining our understanding and improving approaches to patient care, moving towards more individualized interventions.
The Role of Early Diagnosis and Advanced Oncology
Early diagnosis is a critical factor in improving outcomes for pancreatic conditions. Advances in diagnostic imaging, such as MRI and endoscopic ultrasound, along with the development of specific biomarkers, are enhancing the ability to detect issues earlier. In the field of oncology, the focus is increasingly on precision medicine. This involves analyzing the unique genetic makeup of a tumor to identify specific mutations or characteristics that can be targeted by particular therapies. This shift moves away from a one-size-fits-all approach, paving the way for more effective treatment strategies tailored to the individual patient.
Innovations in Therapy and Treatment Approaches
Modern therapy for pancreatic cancer encompasses a range of options, often used in combination. Surgical techniques have become more refined, allowing for better tumor removal in suitable candidates. Chemotherapy remains a cornerstone, but newer regimens and drug combinations are continually being developed to enhance efficacy and reduce side effects. Radiation therapy also plays a role, sometimes used before or after surgery, or for symptom management. Beyond these traditional methods, immunotherapy, which harnesses the body’s immune system to fight cancer, and targeted therapies, which block specific molecules involved in cancer growth, represent significant innovations in treatment. These approaches are often guided by the detailed diagnosis of a patient’s specific disease characteristics.
Comprehensive Patient Care and Support Systems
Effective management of pancreatic health extends beyond medical treatment to encompass holistic patient care. This includes nutritional support, as pancreatic conditions can significantly impact digestion and nutrient absorption. Pain management is also a crucial component, ensuring comfort and improving daily functioning. Psychological and emotional support are equally important, helping patients and their families cope with the challenges of illness. Support groups, counseling services, and palliative care teams play a vital role in providing this comprehensive framework, addressing the physical, emotional, and social needs of individuals navigating their health journey.
Research and Clinical Studies Driving Advances
Ongoing research is fundamental to improving long-term survival and quality of life for individuals with pancreatic conditions. Clinical studies are instrumental in testing new drugs, surgical techniques, and combinations of therapies. These studies allow researchers to gather data on efficacy and safety, ultimately leading to new approved treatments. Participation in clinical trials can offer patients access to cutting-edge interventions that may not yet be widely available. The continuous pursuit of scientific innovation in this area provides hope for future breakthroughs and more effective management strategies.
Understanding Management and Wellness Interventions
Managing pancreatic health involves a long-term perspective focused on wellness. This includes careful monitoring for recurrence, managing side effects of past treatments, and adopting lifestyle adjustments that support overall health. Nutritional guidance from dietitians can help maintain strength and manage digestive issues. Physical activity, tailored to individual capabilities, can improve energy levels and mood. Furthermore, regular follow-up appointments with healthcare providers are essential for ongoing assessment and adjustment of the care plan. The goal is not just to treat the disease but to foster a sustained state of well-being.
Pancreatic health management is a complex but evolving field, with a clear trend towards personalized strategies. By integrating early diagnosis, advanced therapies, comprehensive patient care, and continuous research, the aim is to enhance individual outcomes and improve the overall quality of life for those affected. The journey involves a collaborative effort between patients, their families, and a dedicated healthcare team, focusing on proactive management and sustained wellness.




