Recognizing Signs of a Lung Blood Clot
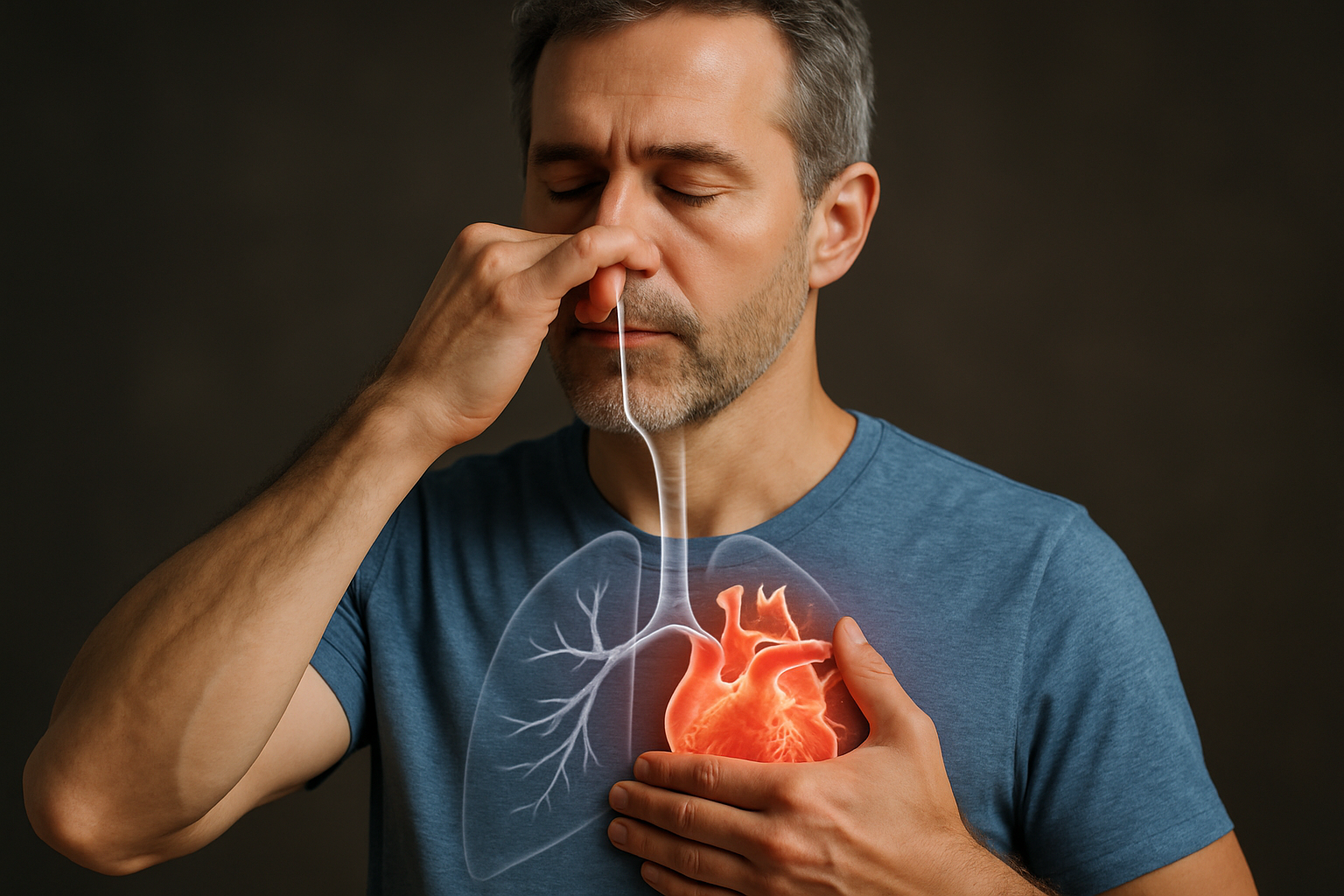
A lung blood clot, medically known as a pulmonary embolism, is a serious condition that occurs when a blood clot travels to the lungs and blocks an artery. This blockage can disrupt blood flow and oxygenation, potentially leading to severe complications if not addressed promptly. Understanding the indicators associated with this vascular event is crucial for timely medical intervention and improving outcomes.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What is a Pulmonary Embolism and How Does it Affect the Lungs?
A pulmonary embolism (PE) involves a blood clot, often originating in the deep veins of the legs (deep vein thrombosis or DVT), which then travels through the circulatory system to the lungs. Once in the lungs, this clot can become lodged in a pulmonary artery, causing a blockage. This interruption to the vascular system prevents blood from reaching parts of the lung, impairing the exchange of oxygen and carbon dioxide, which is vital for overall health.
The severity of a PE depends on the size of the clot and the extent of the artery blockage. A large clot can significantly impede blood flow, leading to a sudden and dangerous drop in oxygenation levels throughout the body. Even smaller clots can cause distress and damage over time, highlighting the importance of early detection and treatment.
Key Indicators of a Lung Blood Clot
Recognizing the signs of a lung blood clot is paramount, as symptoms can sometimes be subtle or mimic other conditions. The most common respiratory symptom is sudden shortness of breathing, which often appears without warning and may worsen with exertion. Chest pain is another frequent indicator, typically sharp or stabbing, and may intensify when taking a deep breath, coughing, or bending over. This pain is often confused with heart-related issues.
Other signs can include a cough that may produce blood-streaked sputum, rapid heart rate, lightheadedness or dizziness, and excessive sweating. In some cases, individuals might experience anxiety or a feeling of impending doom. Swelling, pain, or tenderness in one leg, particularly in the calf or thigh, can also be a significant clue, as it may indicate an underlying deep vein thrombosis (DVT) that is the source of the clot. Any combination of these symptoms warrants immediate medical attention as an emergency.
Understanding Risk Factors for Pulmonary Embolism
Several factors can increase an individual’s risk of developing a pulmonary embolism. Prolonged immobility, such as during long flights, car rides, or extended bed rest after surgery or illness, is a primary risk factor because it slows blood flow, increasing the likelihood of clot formation. Major surgery, especially orthopedic procedures involving the hips or knees, also significantly elevates risk.
Certain health conditions, including cancer and its treatment, heart failure, and inherited blood clotting disorders (thrombophilia), predispose individuals to thrombosis. Pregnancy and the postpartum period, obesity, smoking, and the use of estrogen-containing medications (like oral contraceptives or hormone replacement therapy) are additional factors that can increase the risk of blood clots in the vascular system. A family history of blood clots also plays a role in an individual’s susceptibility.
How is a Lung Blood Clot Diagnosed?
Accurate diagnosis of a lung blood clot requires a comprehensive medical evaluation. When symptoms suggest a PE, healthcare professionals typically begin with a physical examination, reviewing medical history, and assessing risk factors. Initial tests may include blood tests, such as a D-dimer test, which can indicate the presence of blood clots but is not definitive for PE.
Imaging tests are crucial for confirming a diagnosis. A computed tomography pulmonary angiography (CTPA) is often the gold standard, providing detailed images of the pulmonary arteries to detect blockages. Other tests may include a ventilation-perfusion (V/Q) scan, ultrasound of the legs to check for DVT, or an echocardiogram to assess heart strain. The choice of diagnosis method depends on the patient’s condition and the specific clinical context.
Approaches to Treating Pulmonary Embolism
Treatment for a pulmonary embolism typically focuses on preventing the existing clot from growing, stopping new clots from forming, and restoring blood flow to the lungs. Anticoagulant medications, commonly known as blood thinners, are the cornerstone of treatment. These medications do not dissolve existing clots but help prevent their enlargement and the formation of new clots, allowing the body’s natural processes to gradually break down the existing clot.
In more severe cases, particularly when oxygenation is severely compromised or the patient is unstable, stronger interventions may be necessary. Thrombolytic drugs, sometimes called clot busters, can rapidly dissolve clots but carry a higher risk of bleeding. Surgical removal of the clot (pulmonary embolectomy) or placement of a vena cava filter to prevent clots from reaching the lungs may also be considered in specific circumstances. Treatment plans are highly individualized and depend on the clot size, patient health, and other factors.
Prevention Strategies and Public Awareness
Preventing pulmonary embolism involves addressing the underlying risk factors. For individuals at high risk, such as those undergoing surgery or with prolonged immobility, preventive measures are often implemented. These can include early mobilization, wearing compression stockings, and using pneumatic compression devices to promote blood flow in the legs. Prophylactic anticoagulation may also be prescribed in certain high-risk situations.
Public awareness about the signs, symptoms, and prevention of blood clots is vital. Understanding the importance of staying active, especially during long periods of sitting, and recognizing when to seek medical attention for symptoms like sudden shortness of breathing or unexplained chest pain can significantly improve outcomes. Regular health check-ups and open communication with healthcare providers about circulatory health concerns are key components of effective prevention.
Recognizing the signs of a lung blood clot is a critical step in managing this potentially life-threatening condition. Prompt medical evaluation and diagnosis are essential for initiating appropriate treatment and improving patient outcomes. Understanding the risk factors and implementing prevention strategies can help reduce the incidence of pulmonary embolism and its serious health consequences.




