Remote monitoring strategies to track functional improvement
Remote monitoring offers structured ways to observe patient progress outside the clinic, using data from wearable sensors, video assessments, and patient-reported measures to track rehabilitation milestones. By combining objective measures of mobility, gait, strength, and endurance with subjective reports of pain, posture, and function, clinicians can adjust exercise plans and guide recovery remotely.
Remote monitoring strategies to track functional improvement
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Rehabilitation and remote tracking
Remote monitoring can extend rehabilitation beyond scheduled visits by collecting continuous or periodic data on a patient’s activity and functional capacity. Clinicians can use wearable accelerometers, step counters, and app-based check-ins to quantify movement patterns and adherence to exercise programs. These objective data help evaluate progress in mobility and recovery, enabling tailored adjustments that reflect real-world performance rather than only clinic-based observations.
Exercise adherence and feedback
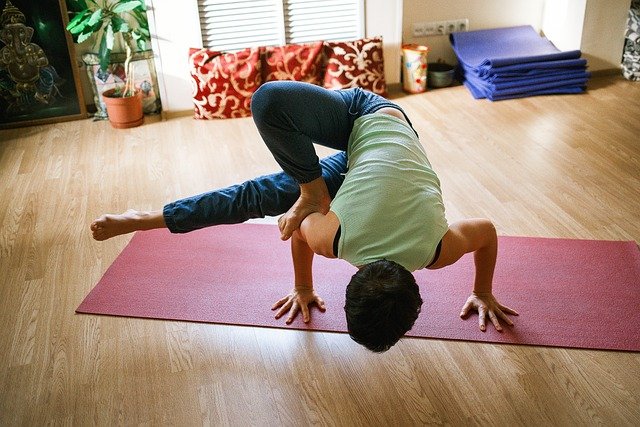
Maintaining consistent exercise is central to recovery. Remote systems can prompt patients with reminders, demonstrate exercises through video, and record completed sessions for clinician review. Feedback loops—such as automated performance scores, clinician comments, or gamified milestones—support engagement while also providing measurable metrics related to strength, flexibility, and endurance. These metrics enable clinicians to compare expected versus actual exercise loads and modify programs to reduce pain or slow progress.
Mobility, gait, and biomechanics
Gait and biomechanics are commonly monitored remotely using smartphone sensors, inertial measurement units, or video analysis tools. These methods can detect changes in stride length, cadence, symmetry, and joint angles that indicate improvements or compensations. Tracking such parameters over time supports assessments of functional mobility and helps identify when targeted interventions—gait retraining, orthotic adjustments, or neuromuscular exercise—are needed to improve overall movement quality.
Pain, posture, and ergonomics
Patient-reported pain scales and posture photos or video allow clinicians to monitor subjective symptoms alongside objective measures. Remote ergonomic assessments—where patients record workstation setups or submit posture images—help identify environmental contributors to pain or impaired recovery. Combining subjective pain reports with objective posture and movement data gives a fuller picture, allowing more precise recommendations for activity modification, home exercise, or ergonomic changes.
Strength, flexibility, balance, and endurance
Measurement approaches for these domains vary: strength can be estimated through functional tasks or instrumented sensors; flexibility through range-of-motion videos; balance through timed tests or sway metrics captured by wearables; endurance through timed walks or activity volume tracking. Remote platforms that integrate multiple measures enable clinicians to monitor improvements across domains, ensuring that gains in strength are translating to better balance or longer walking tolerance, rather than isolated improvements that don’t affect daily function.
Evaluation, neuromuscular monitoring, and outcomes
Evaluative tools for neuromuscular performance—such as electromyography-enabled wearables or clinician-scored functional tests recorded remotely—help detect changes in muscle activation and coordination. Outcome monitoring should include standardized functional measures (timed up-and-go, 6-minute walk equivalents) adapted for remote use, combined with regular clinician evaluation of data trends. This approach supports evidence-based decisions about progression, discharge readiness, or the need for in-person reassessment.
Conclusion
Remote monitoring strategies can complement in-person physiotherapy by providing continuous insight into rehabilitation, exercise adherence, mobility patterns, pain levels, posture, balance, strength, flexibility, endurance, and neuromuscular function. When integrated thoughtfully into care plans, these data-driven approaches support nuanced evaluation and timely adjustments to treatment, improving alignment between clinic goals and everyday function.




