Edema Treatment: Approaches for Eye and Systemic Swelling
Edema describes abnormal fluid accumulation in tissues and can affect many parts of the body, including the eye. Treatment depends on the cause, location and severity; options range from lifestyle changes and medications to targeted medical procedures. Understanding how edema affects vision and overall health helps patients and clinicians choose appropriate, monitored therapies and follow up to reduce complications and preserve function.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What is edema affecting the eye?
Edema in the eye typically refers to swelling within ocular tissues such as the cornea, retina or macula. Macular edema and retinal edema occur when fluid leaks into retinal layers, disrupting the fine architecture responsible for central vision. Causes include diabetic damage to blood vessels, retinal vein occlusions, inflammation (uveitis), post-surgical changes, and certain medications. Symptoms can be subtle at first — blurred or wavy central vision, reduced contrast sensitivity, or a feeling that colors are less vivid. Early detection often preserves better vision outcomes.
How does edema impact vision and the retina?
Retinal and macular edema directly interfere with the retina’s ability to convert light into clear images. When fluid separates or distorts photoreceptor cells, sharp central vision declines and straight lines may appear curved. Chronic edema can lead to permanent structural changes in the retina, increasing the risk of lasting vision loss. Diagnostic imaging such as optical coherence tomography (OCT) and fluorescein angiography are commonly used in medical practice to map fluid location, quantify thickness, and monitor response to treatment. Regular monitoring guides decisions about continued therapy.
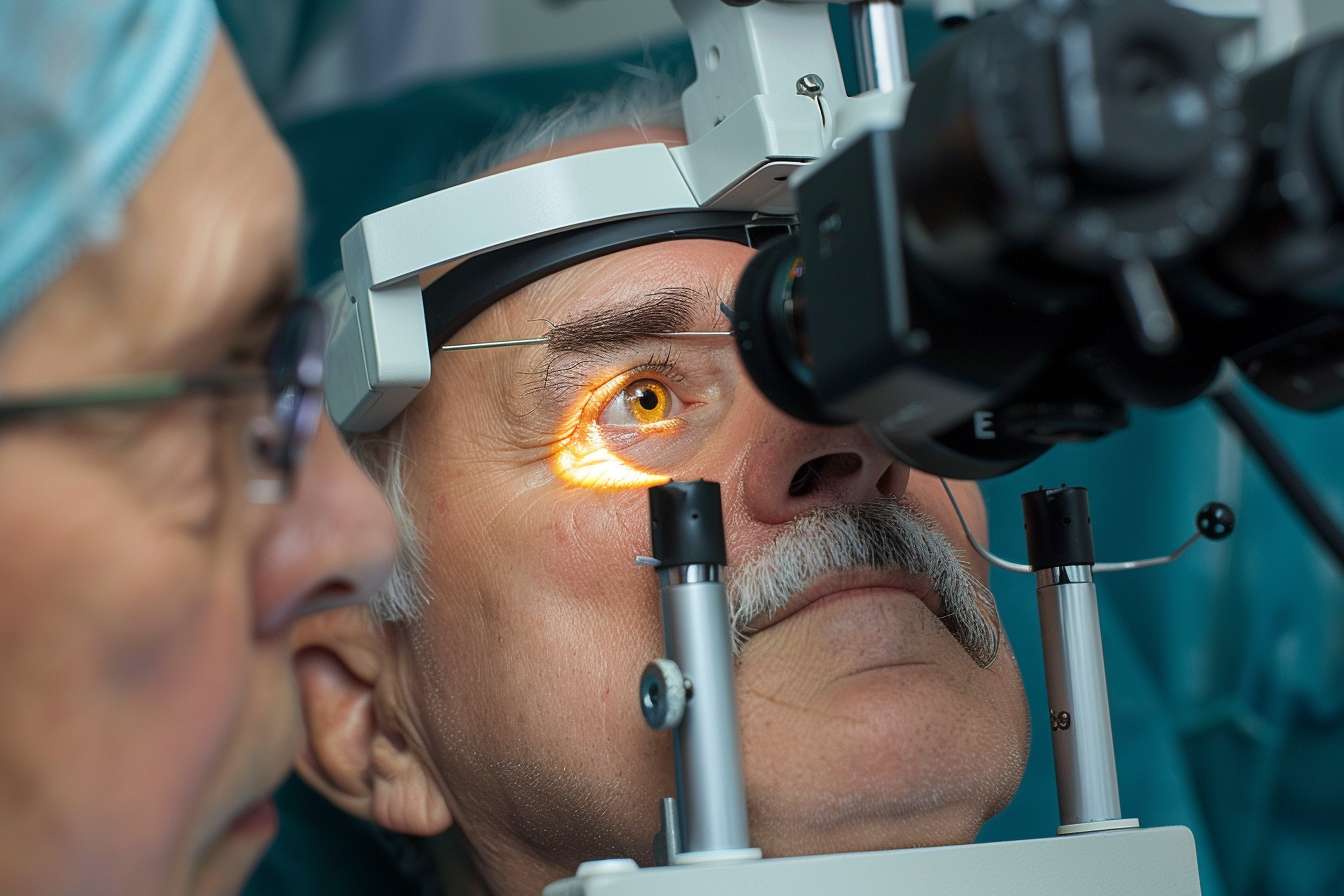
Common medical treatments for ocular edema
Medical management targets the underlying mechanism: reducing leakage, inflammation, or vascular growth factors. Anti-VEGF injections are widely used to treat diabetic macular edema and edema from retinal vein occlusion; they limit abnormal vessel permeability and growth. Corticosteroid eye drops, injections, or implants reduce inflammation and can be effective when inflammation is a dominant factor. Laser photocoagulation remains an option for focal leakage in some cases. In situations where vitreous traction contributes to swelling, surgical vitrectomy may be considered. Each approach has benefits and potential side effects that physicians discuss with patients.
Lifestyle and health measures for edema management
Systemic health control plays a crucial role, particularly when diabetes, high blood pressure, or kidney disease contribute to swelling. Tight blood glucose control, blood pressure management, smoking cessation, and maintaining a healthy weight help reduce the likelihood or severity of edema that affects the eye as well as general health. For peripheral edema (legs, ankles), elevation, compression garments and salt moderation may provide symptomatic relief. Coordinating care between eye specialists and primary care or endocrine teams improves outcomes and addresses root causes rather than only treating local symptoms.
When to seek local services for eye edema
If you notice new blurring, distortion, or changes in central vision, prompt evaluation by an eye care professional is important. Ophthalmologists and retinal specialists provide diagnostic imaging (OCT) and can recommend or administer medical treatments such as intravitreal injections or laser. Local services in your area may include hospital ophthalmology departments, private retinal clinics, or community eye centers; many offer diagnostic testing and follow-up care. Ask about expected monitoring frequency and how treatment responses will be assessed to ensure consistent management.
Conclusion
Edema treatment varies by cause and location — from targeted medical therapies for retinal swelling to systemic measures addressing underlying disease. Early diagnosis using imaging tools, a combination of medical and lifestyle strategies, and coordinated care among specialists and primary providers improve the chance of preserving vision and reducing recurrence. Decisions about interventions should be individualized and made in consultation with qualified healthcare professionals who can explain risks, benefits and monitoring needs.





