Effective Back Pain Treatment: Recovery Strategies and Care
Back pain affects millions worldwide and ranges from a brief twinge after lifting to persistent pain that limits daily life. Understanding practical, evidence-based options helps people make informed choices about treatment, recovery timelines, and when to seek professional care. This article outlines common causes, conservative approaches, and how to work with healthcare professionals to build an effective plan.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Back pain: causes and early steps
Most episodes of back pain stem from muscle strain, overuse, poor posture, or mechanical issues in the spine such as disc degeneration. Acute injuries and sudden movements can trigger sharp pain, while chronic conditions often develop gradually. Early steps typically include modest activity modification, ice or heat for symptom relief, and over-the-counter anti-inflammatory medications when appropriate. Rest beyond a day or two is generally discouraged because prolonged inactivity can slow recovery and weaken supportive musculature.
If pain is accompanied by numbness, weakness in the legs, bowel or bladder changes, or severe progressive symptoms, immediate medical assessment is important to rule out serious causes that may require urgent intervention.
What is physical therapy and how it helps
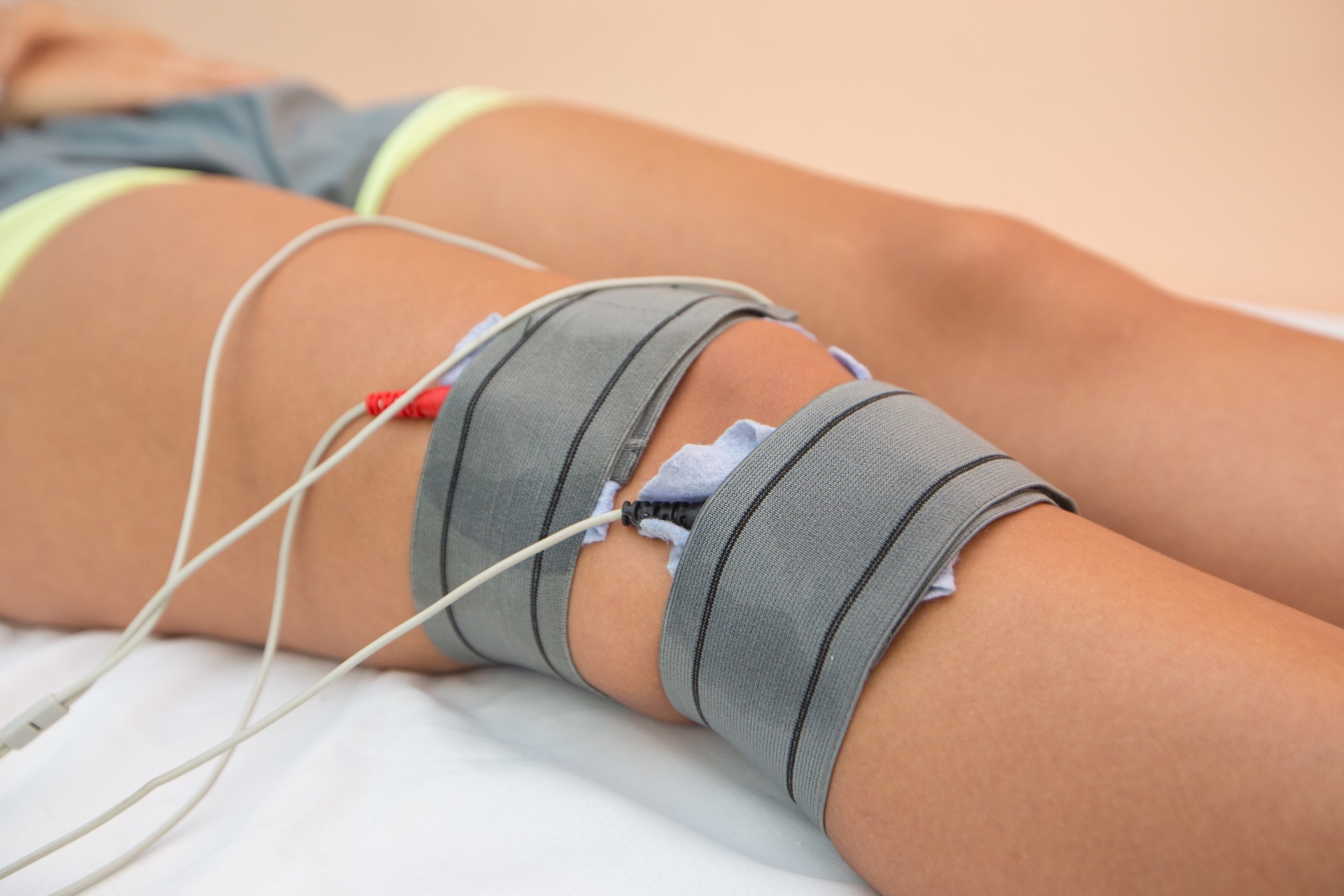
Physical therapy focuses on restoring movement, reducing pain, and preventing recurrence through tailored exercise, manual techniques, and education. A physical therapist evaluates movement patterns, identifies muscle imbalances, and prescribes progressive strengthening and mobility exercises for the core, hips, and back. Therapeutic approaches may include hands-on mobilization, posture training, and modalities like TENS or ultrasound in some settings.
Regular guided sessions combined with a home exercise program improve function and support long-term behavioral changes. Many people experience reduced pain and faster return to daily activities when physical therapy is started early in the recovery process under professional guidance.
Healthcare approaches beyond therapy
Healthcare for back pain spans primary care, pain management, chiropractic care, and specialty services like orthopedics or neurosurgery when needed. Primary care providers often coordinate initial evaluation, imaging decisions, and conservative treatment. Pain specialists may offer injection therapies for targeted relief in selected cases, and surgical consultation is reserved for specific structural problems or severe neurological compromise.
Multidisciplinary clinics can provide combined services—physical therapy, behavioral health, and medical management—especially valuable for chronic pain where psychosocial factors influence recovery. Choosing providers who communicate and collaborate can streamline care and reduce unnecessary tests or treatments.
Choosing the right treatment plan
An effective treatment plan balances symptom relief with functional goals. Conservative care—activity modification, guided exercise, education, and short-term medication—resolves most back pain episodes. Treatment selection should consider pain severity, imaging findings (when appropriate), personal health history, and patient preferences. For chronic or recurrent pain, cognitive behavioral approaches and graded activity programs often complement physical interventions to address fear-avoidance and improve resilience.
Periodic reassessment is important: if a structured conservative plan does not yield progress after a reasonable period (usually several weeks to a few months depending on severity), escalation to specialist evaluation or additional diagnostics may be warranted.
Strategies to support recovery at home
Home strategies accelerate recovery and reduce recurrence risk. Focus on consistent core and glute strengthening, gentle mobility work, and incorporating ergonomic adjustments at work and home. Simple habits—maintaining an active routine, spreading tasks to avoid sustained positions, using proper lifting mechanics, and sleeping with supportive mattresses or pillows—matter. Weight management and cardiovascular fitness also reduce mechanical stress on the spine and improve resilience.
Self-care must be balanced with professional guidance; if exercises increase severe pain or produce new neurological symptoms, stop and consult your healthcare provider or physical therapist.
Conclusion
Back pain treatment is most effective when tailored, progressive, and guided by qualified professionals who consider the whole person: physical function, lifestyle, and goals for recovery. Conservative measures including physical therapy, patient education, and coordinated healthcare often resolve symptoms and prevent recurrence. For persistent or severe cases, structured reassessment and specialist input help determine appropriate further interventions. Prioritizing movement, posture, and consistent self-care supports long-term spinal health and functional recovery.






