Gene Therapy Treatment for Arthritis: Current Science and Trials
Gene therapy uses molecular tools to alter gene expression with the goal of preventing or reversing disease processes. In the context of arthritis, researchers are investigating ways to reduce inflammation, regenerate joint tissue, or modulate immune responses by delivering therapeutic genes to affected cells. Progress combines laboratory studies, animal models, and early human clinical trials. This article explains the scientific approach, the role of stem cells, the state of medical research, how clinical trials are designed, and safety considerations for gene-based therapies.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Gene therapy and arthritis
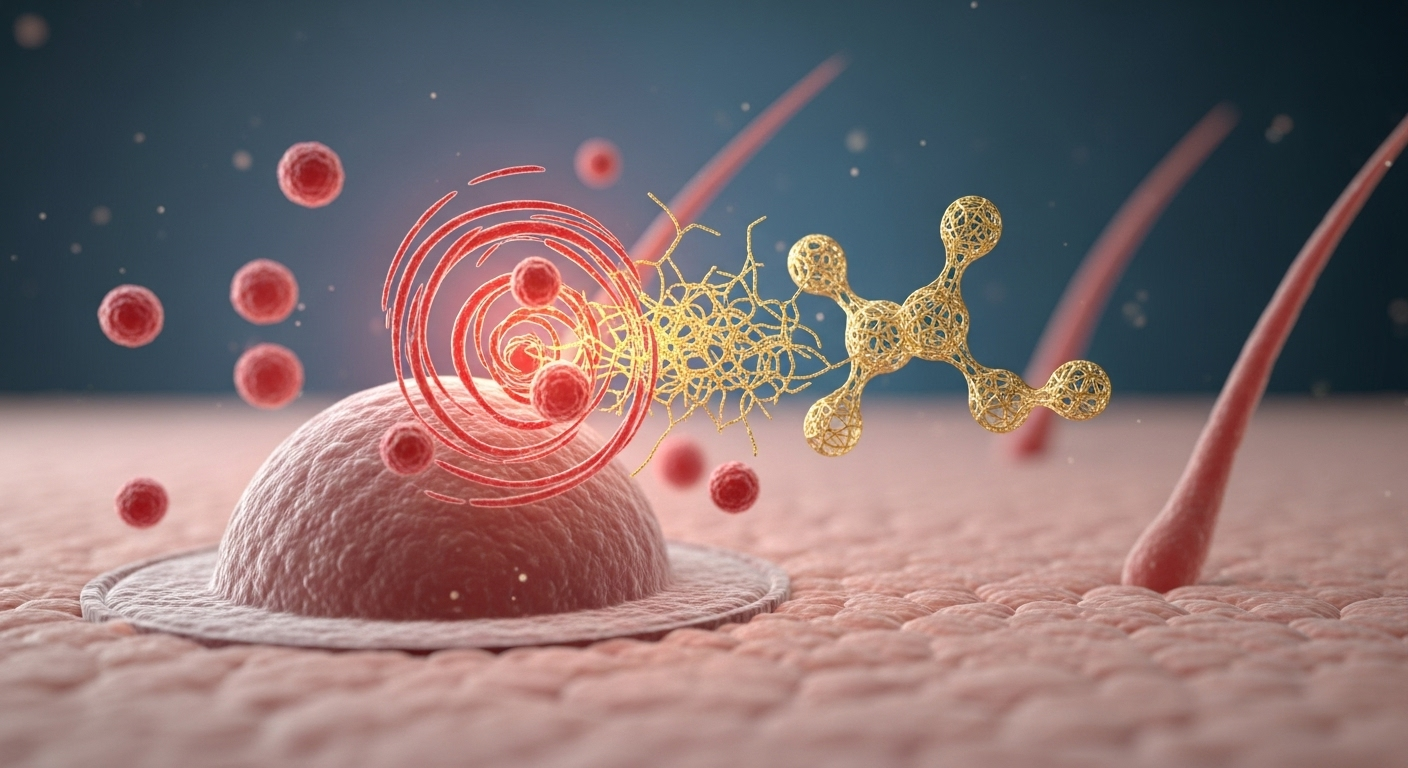
Gene-based strategies for arthritis focus mainly on osteoarthritis and inflammatory forms such as rheumatoid arthritis. Approaches include intra-articular delivery of genes that encode anti-inflammatory proteins or growth factors intended to reduce pain and slow cartilage breakdown. Some therapies aim to provide a sustained local source of a therapeutic protein, avoiding repeated injections of biologics. Current research shows promising biological effects in lab and animal studies, but widespread clinical approval for routine treatment of arthritis has not yet been achieved.
Stem cells in gene-based approaches
Stem cells are studied both as a direct regenerative option and as vehicles for gene delivery. Mesenchymal stem cells (MSCs) can be engineered ex vivo to express therapeutic genes before being implanted into a joint, combining cellular repair potential with targeted molecular effects. This hybrid approach may enhance tissue repair and modulate local immune responses. However, the distinction between stem cell therapy and gene therapy is important: one provides cells with intrinsic properties, while gene approaches modify specific molecular pathways. Both areas remain under active clinical investigation.
Medical research progress and findings
Medical research into gene therapy for arthritis spans molecular biology, vector engineering, and translational studies. Investigators are refining viral and nonviral delivery systems to achieve durable expression while minimizing immune reactions. Preclinical work has established proof-of-concept for several targets, such as cytokine inhibitors and anabolic growth factors. Peer-reviewed studies report variable outcomes across species and models, highlighting the need for rigorous replication and well-controlled human trials. Regulatory frameworks require demonstration of safety and consistent manufacturing before therapies can move toward approval.
Clinical trials: design and stages
Clinical trials for gene therapies follow the standard phased pathway: early-phase studies emphasize safety and dosing, while later phases assess efficacy and longer-term outcomes. For arthritis-related gene trials, common endpoints include pain scores, functional measures, imaging of joint structure, and biomarker changes. Enrollment criteria often restrict participation to specific disease stages or prior treatment histories. Trial designers must balance the need for measurable outcomes with realistic timelines, since structural changes in joints can take months to years to detect. Transparency in trial reporting and independent review are essential.
Safety and long-term therapy outcomes
Safety considerations include immune responses to delivery vectors, off-target effects if gene editing tools are used, and potential for uncontrolled or prolonged expression of therapeutic genes. Long-term monitoring is necessary to detect late adverse events and to determine durability of benefit. Manufacturing consistency and quality control are also critical to ensure predictable dosing and reduce variability between treatments. Regulators typically require post-trial surveillance plans. Patients and clinicians should weigh potential benefits against these uncertainties when considering participation in clinical research or experimental treatments.
Conclusion
Gene therapy for arthritis represents a growing area of medical research that brings together molecular genetics, vector technology, and cell-based methods such as stem cell engineering. Clinical trials are underway to establish whether these approaches can provide sustained symptom relief or structural joint benefit beyond current standards of care. While early results are encouraging in controlled settings, broader clinical adoption depends on demonstrated safety, efficacy, and scalable manufacturing. Individuals interested in emerging therapies should seek information from qualified healthcare professionals and reputable clinical trial registries to explore options available in your area.






