Glaucoma Treatment: Medical Options and Specialist Care
Glaucoma describes a group of eye conditions that damage the optic nerve and can lead to vision loss if untreated. Many people do not notice early symptoms, so diagnosis often comes from routine eye exams. Treatment aims to lower intraocular pressure (IOP) or protect the optic nerve to slow or prevent progression. Options range from topical eye drops and oral medications to laser procedures and surgical interventions performed by trained specialists. Understanding these choices, how they work, and what to expect helps patients work with their doctor to manage the condition effectively.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What is glaucoma and how does it affect the eye?
Glaucoma is not a single disease but a set of conditions that typically involve increased pressure inside the eye or poor blood flow to the optic nerve. The optic nerve transmits visual information to the brain; ongoing damage can cause irreversible peripheral vision loss and, in advanced cases, central vision impairment. Types include open-angle glaucoma (most common), angle-closure glaucoma, normal-tension glaucoma, and secondary glaucomas related to injury or other eye diseases. Regular eye examinations by an eye doctor can detect early signs such as optic nerve changes, visual field defects, or elevated eye pressure.
When should you see an eye doctor for glaucoma?
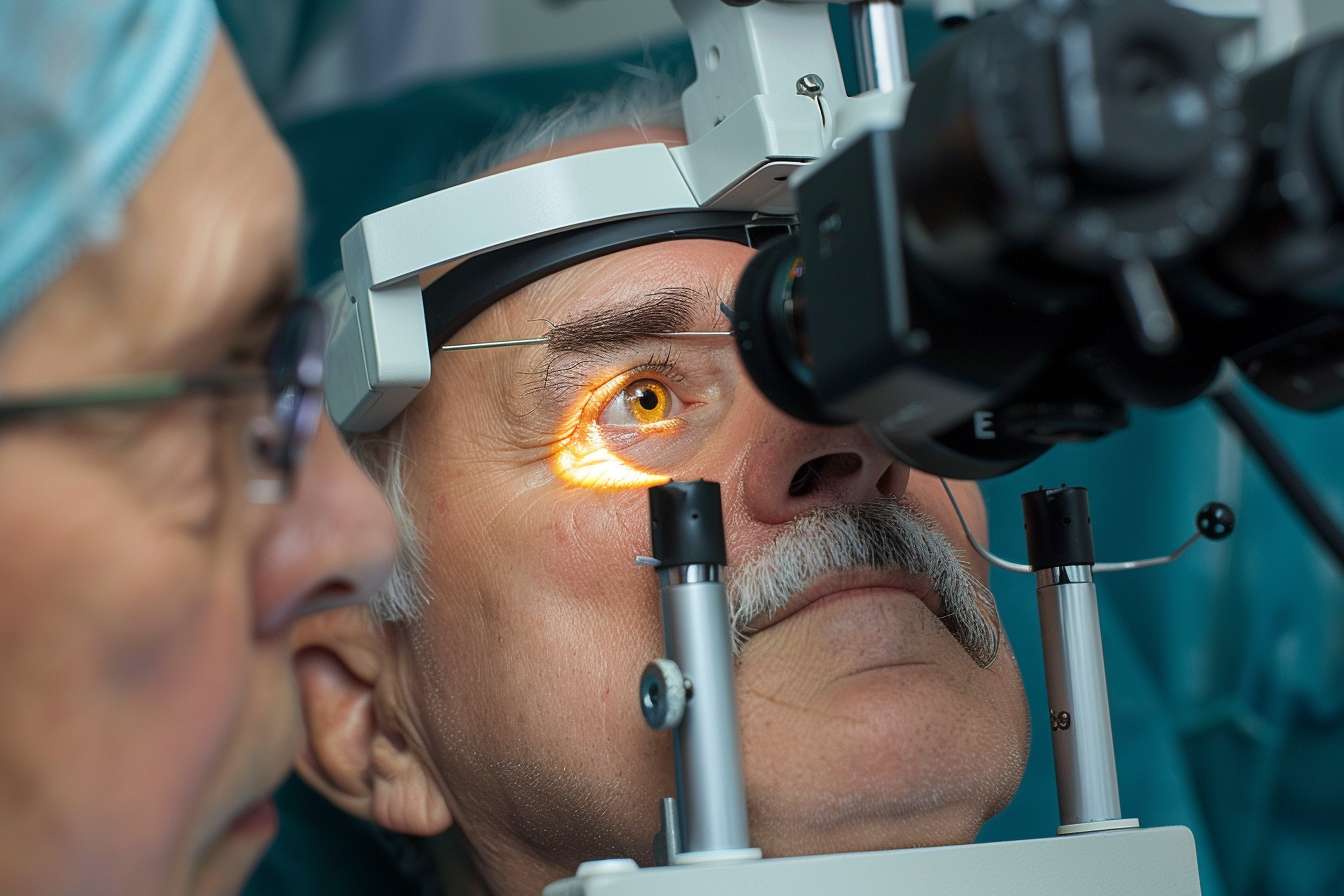
Routine screening is especially important for people with risk factors: age over 60, a family history of glaucoma, high myopia, certain ethnic backgrounds, or systemic conditions like diabetes and hypertension. Symptoms of acute angle-closure glaucoma (severe eye pain, headache, nausea, sudden vision loss) require immediate medical attention. For chronic forms, symptoms may be subtle or absent early on, so follow-up visits with a qualified eye specialist for pressure checks, optic nerve imaging, and visual field testing are central to timely detection and management.
What medical treatments are available for glaucoma?
First-line medical therapy commonly involves topical eye drops that lower intraocular pressure by reducing fluid production or increasing fluid outflow. Classes include prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors. Oral medications may be used temporarily in certain situations. Medical treatments require adherence — missing doses can reduce effectiveness. Side effects vary by drug class and may affect the eye (redness, irritation) or the whole body (cardiovascular or respiratory effects with some beta-blockers), so discussing medical history and concurrent medications with your doctor is important.
What surgical or laser options might a specialist offer?
When medications and laser therapy are insufficient or not tolerated, surgical options are considered. Laser trabeculoplasty can improve drainage in open-angle glaucoma and is often performed in an outpatient setting. Minimally invasive glaucoma surgeries (MIGS) offer lower-risk surgical alternatives designed to enhance outflow pathways and are frequently combined with cataract surgery. Traditional filtering surgeries (trabeculectomy) and tube shunt implants create new pathways for aqueous humor to exit the eye; these are generally reserved for more advanced or refractory glaucoma. Each approach has different risk profiles and recovery expectations; a glaucoma specialist will recommend the most appropriate procedure based on disease severity, anatomy, and overall health.
How is long-term specialist care and monitoring managed?
Glaucoma is typically a chronic condition requiring lifelong monitoring. Care plans include scheduled visits for intraocular pressure measurement, optic nerve imaging (OCT), and visual field testing to track progression. Medication regimens may change over time, and procedural interventions can be staged according to disease activity. Coordination between the patient, primary care doctor, and eye specialist helps manage systemic factors (blood pressure, blood sugar) that can influence optic nerve health. Education about adherence, recognizing warning signs, and lifestyle factors that support eye health are part of comprehensive management.
Conclusion
Effective glaucoma treatment depends on accurate diagnosis, tailored medical or surgical options, and ongoing monitoring by an eye doctor or glaucoma specialist. Early detection through regular eye examinations increases the chances of slowing disease progression and preserving vision. Treatment choices balance benefits, risks, and patient-specific factors, and they are best determined through shared decision-making with qualified medical professionals.





