Glaucoma Treatment: Options and Roles of Eye Doctors and Specialists
Glaucoma is a group of eye conditions that can damage the optic nerve and lead to vision loss if untreated. Treatment aims to preserve remaining vision, slow or stop progression, and manage contributing factors such as intraocular pressure. Understanding available approaches, what to expect from medical care, and when to consult a specialist helps people and caregivers make informed decisions about long-term eye health.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What is glaucoma and how does it affect the eye?
Glaucoma commonly involves increased pressure inside the eye that harms the optic nerve, though some forms occur with normal pressure. Damage is typically gradual and painless, producing peripheral vision loss before central vision is affected. Early detection matters because structural nerve changes can be measured before noticeable vision changes. Regular comprehensive eye exams that include optic nerve assessment, visual field testing, and intraocular pressure measurement are key tools used by eye care teams to diagnose glaucoma and monitor progression.
When should you see an eye doctor for glaucoma?
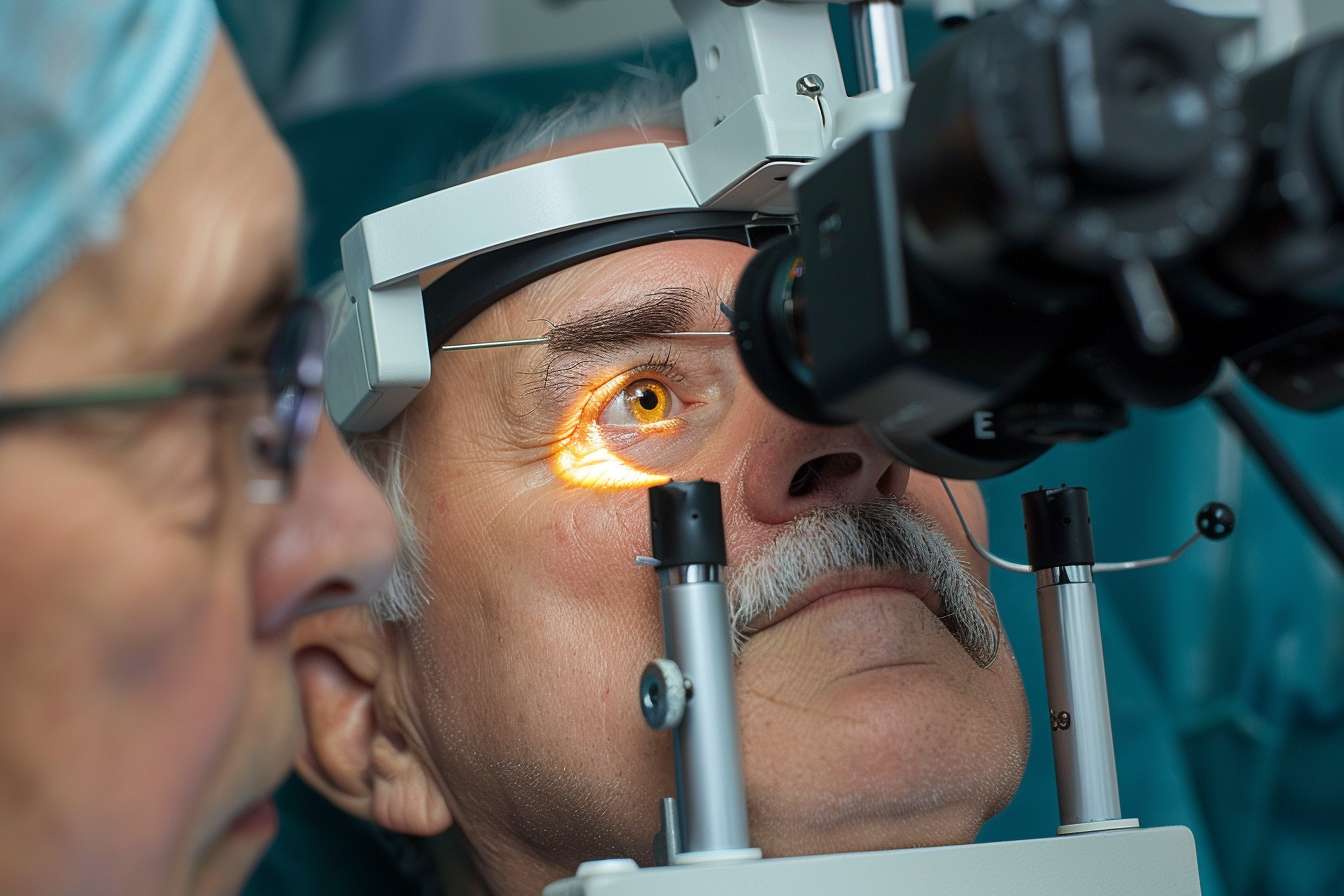
See an eye doctor if you have risk factors such as a family history of glaucoma, older age, certain ethnic backgrounds, high intraocular pressure, or conditions like diabetes. Symptoms that merit prompt evaluation include sudden vision changes, eye pain, halos around lights, or rapid vision loss — though many people have no symptoms in early stages. An eye doctor (optometrist or ophthalmologist) can perform diagnostic testing, interpret results, and recommend appropriate next steps based on your risk profile and exam findings.
What medical treatments are available for glaucoma?
Medical management typically begins with prescription eye drops to lower intraocular pressure by reducing fluid production or increasing drainage. Several drug classes are available; choice depends on effectiveness, side effects, cost, and patient adherence. Oral medications are less commonly used but may be prescribed in acute or refractory cases. Regular monitoring is necessary to assess response and side effects. Medication can preserve vision for many people, but adherence to dosing schedules and follow-up appointments is critical to maintain benefit and detect progression.
Additional medical considerations include managing systemic health factors that can affect glaucoma care, such as blood pressure control and medication interactions. Your doctor will review your overall medical history to choose the safest, most effective regimen.
When is a glaucoma specialist recommended?
A glaucoma specialist—an ophthalmologist with extra training in glaucoma—may be recommended for complex cases, rapidly progressing disease, inadequate response to medications, or when surgical options are being considered. Specialists perform advanced diagnostics (e.g., optical coherence tomography, gonioscopy) and offer interventions such as laser treatments, minimally invasive glaucoma surgeries (MIGS), trabeculectomy, or drainage implant procedures. Referral to a specialist does not always mean immediate surgery; often it ensures tailored management for eyes at higher risk of vision loss.
Monitoring and follow-up care for glaucoma
Ongoing monitoring typically combines pressure checks, optic nerve imaging, and visual field testing at intervals set by disease severity and rate of change. Stable early glaucoma may be seen every 6–12 months, while active or advanced disease requires closer follow-up. Adherence to medications and lifestyle considerations—like avoiding activities that raise eye pressure and managing comorbidities—support long-term outcomes. Family education is also important because first-degree relatives may need screening due to hereditary risk.
When treatment changes occur—new drops, laser, or surgery—post-treatment follow-up is intensified to assess effectiveness and detect complications early.
Conclusion
Glaucoma treatment is individualized and may include medications, laser procedures, or surgery guided by regular monitoring and specialist input when needed. Early detection through routine eye examinations and clear communication with your eye doctor about symptoms, adherence, and medical history are central to preserving vision. Long-term management focuses on slowing disease progression and maintaining quality of vision through coordinated medical care.






