Hair Restoration: Procedures, Options, and Expectations
Hair restoration covers a range of approaches people use to address thinning or lost hair, from medical treatments to surgical procedures. This article explains common causes, how professionals evaluate hair changes, available medical and non-surgical options, and how treatment plans are selected so you can make informed decisions about care in your area.
Hair: common causes of thinning and loss
Hair health is influenced by genetics, hormones, age, nutrition, and environmental factors. Androgenetic alopecia (pattern hair loss) is the most frequent cause in adults, but conditions such as telogen effluvium, autoimmune alopecia areata, scalp infections, and certain medications can also lead to diminished hair density. Lifestyle elements — stress, diet, and hair styling practices — can accelerate shedding or damage hair shafts. Identifying the underlying cause is important because it directs whether the approach should focus on preventing further loss, stimulating regrowth, or replacing hair surgically.
Hair restoration: non-surgical and surgical approaches
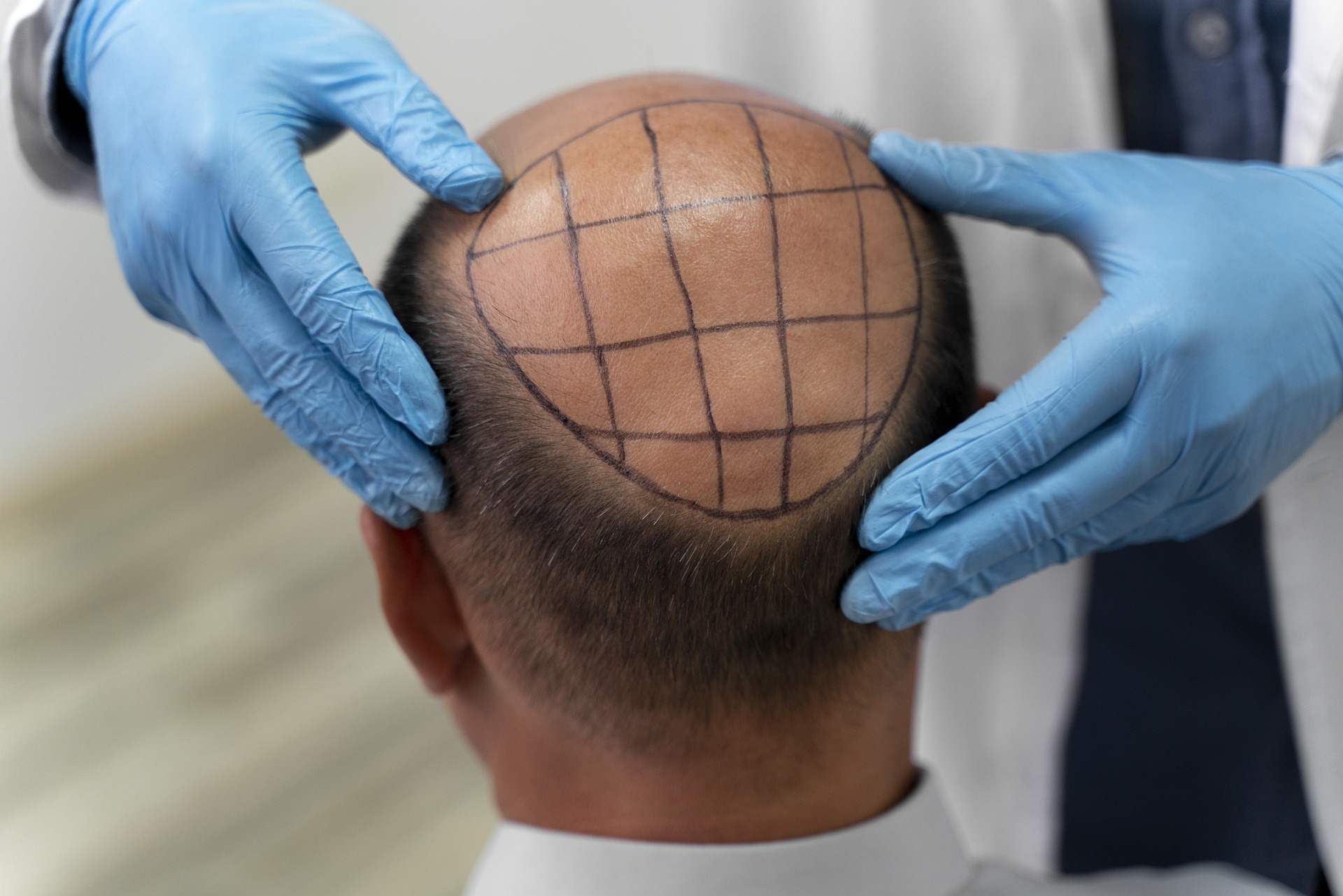
Hair restoration spans topical and oral medications, light-based therapies, platelet-rich plasma, and hair transplant surgery. Minoxidil and finasteride are commonly prescribed treatments aimed at slowing hair loss and sometimes encouraging regrowth. Low-level laser therapy and PRP are offered as adjuncts intended to improve scalp environment and follicle function. Surgical options such as follicular unit extraction (FUE) and follicular unit transplantation (FUT) relocate hair-bearing tissue to thinning areas. Choice of approach depends on the diagnosis, extent of loss, donor hair availability, and patient expectations.
Hair loss: evaluation and diagnostic steps
A thorough evaluation starts with medical history, pattern and timeline of hair loss, family history, and medication review. A clinician performs scalp examination, sometimes using dermoscopy to inspect follicles, and may order blood tests to check thyroid function, iron levels, or hormonal contributors. Scalp biopsy is occasionally used when diagnosis is unclear. Accurate diagnosis helps avoid ineffective treatments and allows targeted plans — for example, treating an underlying thyroid disorder can reverse hair loss from that cause, while pattern hair loss may require long-term medical or surgical strategies.
Medical procedure: surgical and non-surgical considerations
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment. Surgical hair restoration is a medical procedure that requires preoperative assessment, sterile technique, and postoperative care. FUE harvests individual follicular units and typically leaves small dot scars, whereas FUT removes a strip of scalp and produces a linear scar. Both carry risks such as infection, scarring, and variable graft survival. Non-surgical procedures (e.g., PRP, topical agents) usually have lower immediate risk but may require ongoing use and periodic maintenance sessions to sustain results.
Treatment: tailoring a plan and expected timelines
A realistic treatment plan aligns patient goals with clinical findings. Medical treatments often take months to show measurable results; most clinicians expect initial changes in three to six months and clearer improvement at 9–12 months. Surgical restoration provides more immediate density changes once grafts take, but full maturation of transplanted hair can take up to 12–18 months. Combining treatments—medical therapy before and after surgery, plus supportive options like PRP—can help preserve native hair and enhance outcomes. Follow-up and adherence are important; clinicians monitor progress and adjust the treatment plan if needed.
Local services: choosing qualified providers in your area
When seeking hair restoration services locally, prioritize board-certified dermatologists, hair restoration surgeons with appropriate training, or clinics affiliated with recognized professional societies. Review providers’ clinical photos (with explanation of typical timelines), ask about the team’s experience with specific procedures, and inquire how postoperative care and complications are managed. Teleconsultations can help screen options before in-person visits, but an on-site evaluation is often necessary for accurate assessment. Look for transparent communication about risks, expected outcomes, and maintenance requirements.
This article summarizes common approaches to hair restoration and how professionals assess and treat hair loss. Individual needs and responses vary, so diagnostic clarity and a tailored plan are central to effective care. Consulting qualified clinicians ensures appropriate evaluation of causes, selection of suitable medical procedures or treatments, and realistic expectations about timelines and outcomes.




