Managing Kidney Disease: Treatments, Choices & Advances
Kidney disease demands a careful, multi-pronged approach to preserve function and quality of life. This article breaks down lifestyle steps, medications, dialysis options, transplantation, and promising new therapies—helping patients and caregivers understand treatment choices, timing, and what to expect.

Kidney disease requires a coordinated strategy combining lifestyle changes, medical therapies, and sometimes procedural interventions. Understanding the available options—when they are used and how they work—helps people living with kidney disease make informed decisions with their healthcare team.
The impact of lifestyle changes on kidney health
Lifestyle adjustments are foundational for slowing kidney damage and improving overall wellbeing. Dietary guidance commonly includes limiting sodium to control blood pressure and fluid balance, and moderating protein intake to reduce the kidneys’ workload. Depending on lab values and the disease stage, restrictions on potassium and phosphorus may also be necessary to prevent dangerous electrolyte and bone-mineral disturbances.
Regular physical activity, tailored to ability and medical advice, supports cardiovascular health and weight management. Smoking cessation and cutting back on alcohol are important because both can accelerate kidney injury and worsen related conditions such as hypertension and cardiovascular disease. Staying hydrated within recommended limits and avoiding overuse of nonsteroidal anti-inflammatory drugs (NSAIDs) are additional practical steps.
Medical therapies used in treatment
Medication choices depend on the cause and stage of kidney disease as well as coexisting conditions. Common prescriptions include:
- Blood pressure agents: ACE inhibitors and angiotensin receptor blockers (ARBs) are frequently used to control hypertension and offer kidney-protective effects beyond blood pressure lowering.
- Diuretics: These help reduce fluid overload and swelling when kidneys cannot remove excess fluid efficiently.
- Erythropoiesis-stimulating agents (ESAs): Used to treat anemia that often accompanies chronic kidney disease by supporting red blood cell production.
- Phosphate binders and vitamin D: Employed to manage disordered mineral metabolism and protect bone health as kidney function declines.
- Immunosuppressive therapies: In autoimmune or inflammatory kidney diseases, drugs that suppress the immune response may be required to reduce ongoing damage.
Treatment is individualized: doses and drug combinations are adjusted regularly based on laboratory testing, symptoms, and progression.
When dialysis becomes necessary
Dialysis is indicated when waste products and fluid accumulate to dangerous levels and the kidneys can no longer keep pace—commonly when function falls below roughly 10–15% of normal. Dialysis replaces some filtration functions of the kidney and can be life-sustaining.
Two main dialysis modalities are used:
- Hemodialysis: Blood is routed through a machine and filtered outside the body, usually at a center several times per week. It is effective at removing waste and extra fluid.
- Peritoneal dialysis: The peritoneal membrane inside the abdomen serves as the filter; fluid is introduced and drained through a catheter. This method can be performed at home and may offer greater lifestyle flexibility for some patients.
Choosing between these options depends on medical suitability, lifestyle preferences, support systems, and the presence of other health issues. For many, dialysis is a temporary measure while awaiting transplantation; for others it remains long-term therapy.
Kidney transplantation: benefits and considerations
Transplantation is often regarded as the best treatment for end-stage kidney disease because it can restore more normal kidney function, improve quality of life, and offer better long-term survival compared with dialysis for many recipients. Transplants come from living or deceased donors and require careful matching for compatibility.
Transplant candidates must be evaluated for suitability, and patients who receive a kidney must take lifelong immunosuppressive medications to prevent rejection. These drugs reduce immune response but increase infection risk, so ongoing monitoring and follow-up care are essential.
Emerging and experimental approaches
Research into kidney disease treatments is active, and several forward-looking strategies are under investigation:
- Regenerative medicine: Studies are exploring the potential for stem cells and tissue engineering to repair damaged renal tissue.
- Gene therapy: Targeting inherited or molecular drivers of specific kidney diseases may allow more precise interventions.
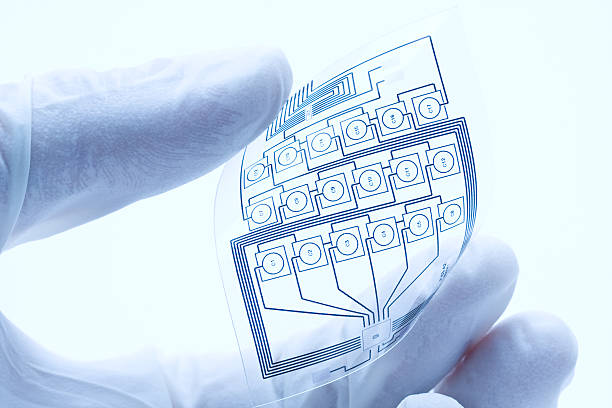
- Artificial and wearable kidneys: Implantable or portable devices aim to mimic natural filtration and reduce dependence on center-based dialysis.
- Precision medicine: Using genetic and molecular profiling to tailor treatments to an individual’s disease subtype and risk profile.
These approaches are at varying stages of clinical testing and may offer more personalized, effective treatments in the future.
| Treatment | Typical schedule or frequency | Approximate cost range (USD) |
|---|---|---|
| Lifestyle and diet counseling | Ongoing | Low to moderate (provider/clinic dependent) |
| Medications (antihypertensives, binders, ESAs) | Daily/regular | Variable (depends on drugs and insurance) |
| Hemodialysis | Usually 3 times weekly | $300–$500 per session (varies widely) |
| Peritoneal dialysis | Daily exchanges | Monthly supplies and training costs (varies) |
| Kidney transplant (surgery + follow-up) | One-time surgery, lifelong meds | High upfront surgical costs; ongoing immunosuppression expenses |
Costs are estimates and vary widely depending on country, healthcare system, provider, and insurance coverage. They are provided for informational purposes only.
Making decisions with your healthcare team
No single pathway fits every person with kidney disease. Timing of interventions, choice of dialysis modality, and candidacy for transplant should be decided collaboratively with nephrologists, transplant teams, dietitians, and primary care providers. Regular monitoring, lab testing, and open communication about goals, preferences, and lifestyle needs are central to effective care.
Advances in medicine continue to expand options, but core principles remain the same: slow progression where possible, manage complications, and align treatment choices with the patient’s life and priorities.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.