Managing Risk Factors for Arterial Blockages
Arterial blockages, often caused by blood clots, represent a significant health concern that can disrupt normal bodily functions and lead to serious complications. Understanding the factors that contribute to these blockages is crucial for maintaining cardiovascular and respiratory health. Proactive management of these risks can play a vital role in preventing severe health events and promoting overall well-being. This article explores various aspects of arterial blockages, from their formation to strategies for prevention and recovery.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Understanding Vascular Blockages and Blood Clot Formation
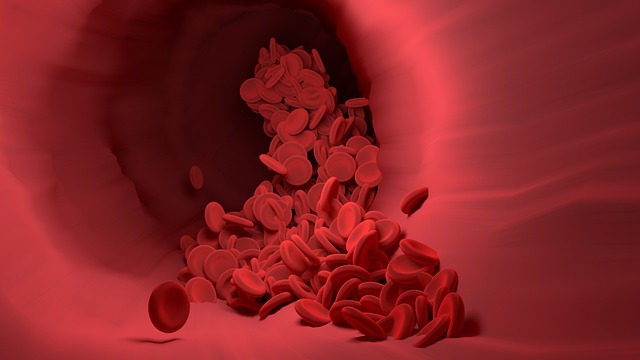
Arterial blockages occur when substances, most commonly blood clots, obstruct the flow of blood through arteries. These clots, a process known as thrombosis, can form in various parts of the body, particularly in the deep veins of the legs, a condition called deep vein thrombosis (DVT). If a piece of this bloodclot breaks off, it can travel through the circulation system, potentially reaching the lungs and causing a blockage that impairs oxygen exchange. Maintaining healthy vascular function is essential to prevent such events, as compromised circulation can increase the likelihood of clot formation within the artery walls.
Recognizing Key Symptoms and Emergency Indicators
Identifying the symptoms associated with arterial blockages is critical for timely intervention. When a blockage affects the lungs, common respiratory symptoms may include sudden shortness of breath, chest pain that worsens with deep breathing, and coughing, sometimes with blood. Other indicators can be lightheadedness, rapid heart rate, or unexplained anxiety. These symptoms often develop suddenly and require immediate medical attention. Understanding these emergency signs can make a significant difference in outcomes, as prompt diagnosis and treatment are vital to restore oxygen supply and prevent further complications.
Strategies for Prevention and Risk Factor Management
Prevention is a cornerstone in managing the risk of developing arterial blockages. Several factors can increase the likelihood of blood clotting, including prolonged immobility, certain medical conditions, surgery, and genetic predispositions. Lifestyle adjustments, such as regular physical activity, maintaining a healthy weight, and avoiding long periods of sitting or standing, can significantly reduce risk. For individuals at higher risk, a healthcare professional might recommend specific preventive measures, such as compression stockings or anticoagulant medications. Regular awareness of personal risk factors and proactive discussions with medical providers are key steps in a comprehensive prevention strategy.
Diagnostic Methods and Treatment Approaches
When symptoms suggest an arterial blockage, healthcare professionals employ various diagnostic tools to confirm the condition. These may include imaging tests like CT pulmonary angiography, ventilation-perfusion scans, or ultrasound to detect deep vein thrombosis. Once diagnosed, treatment typically focuses on dissolving the existing clot and preventing new ones from forming. Medications such as anticoagulants are commonly prescribed to thin the blood, while in more severe cases, thrombolytic drugs may be used to rapidly break down large clots. Surgical interventions or catheter-based procedures might also be considered for specific situations to remove the blockage or improve blood flow.
Long-Term Recovery and Maintaining Health
Following treatment for an arterial blockage, the recovery process involves careful monitoring and ongoing management to ensure long-term health. Patients often require continued anticoagulant therapy for several months or longer, depending on the underlying cause and individual risk factors. Regular follow-up appointments with healthcare providers are essential to assess progress, adjust medication, and manage any residual symptoms or potential complications. Lifestyle modifications, including adherence to a balanced diet, regular exercise, and avoiding smoking, play a crucial role in promoting overall vascular health and minimizing the risk of recurrence. Patient education and self-awareness about potential recurring symptoms are also vital components of a successful recovery journey.




