Medical evaluations that should accompany unexplained visual changes
Unexplained changes in sight—such as sudden blur, increased glare, or altered acuity—warrant timely evaluation. This article outlines the medical assessments clinicians commonly use to investigate visual changes, explains why each is useful, and describes how findings guide further diagnostics and rehabilitation.

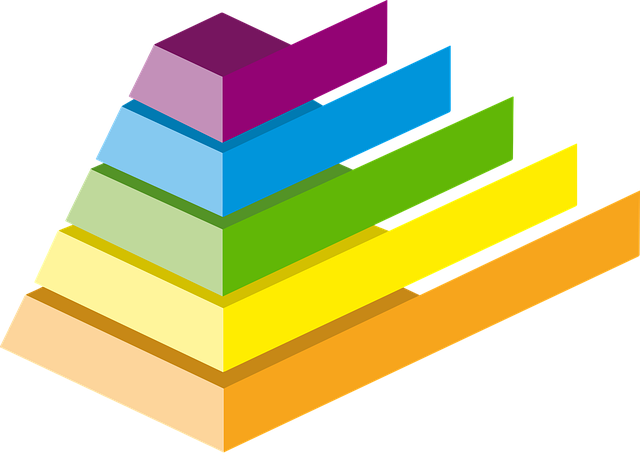
Unexplained visual changes can be unsettling: tasks that used to be straightforward may become difficult when vision shifts, blur appears, or glare worsens. A systematic approach helps identify whether the cause is ocular, neurologic, optical, or related to systemic health. The initial evaluation typically focuses on screening tests and measures of acuity, followed by more specific refraction and optics assessments, targeted imaging, retina and ocular examination, and, where indicated, neurology diagnostics and rehabilitative strategies.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What screening and acuity checks are needed?
Screening and acuity tests form the backbone of an initial assessment. Visual acuity charts quantify central clarity at distance and near, while screening for peripheral fields can reveal deficits suggestive of optic nerve or brain pathway issues. Simple measures—pinhole testing to separate refractive blur from more serious pathology, contrast sensitivity to detect subtle losses, and glare testing for light scatter problems—give clinicians a quick diagnostic roadmap. Documenting baseline acuity and any asymmetry between eyes also helps determine urgency and next steps.
How does refraction and optics assessment help?
A comprehensive refraction evaluates whether uncorrected or changing refractive error explains blur or reduced acuity. Refraction testing identifies spherical, cylindrical, and multifocal needs; lensometry and assessment of current spectacles can show outdated prescriptions. Optics-focused examination includes slit-lamp inspection of the cornea and lens to detect early cataract or irregular astigmatism, both of which increase glare and reduce image quality. When optics alone do not account for symptoms, clinicians broaden the differential to involve retina or neurological causes.
When should imaging and retina evaluation be done?
Ocular imaging is indicated if structural causes are suspected. Optical coherence tomography and fundus photography evaluate the retina and optic nerve; they can detect macular edema, retinal detachments, or optic nerve swelling that produce visual distortion or field loss. Ultrasound and fluorescein angiography are used selectively. Neuroimaging (MRI or CT) becomes important if ocular imaging is normal but symptoms suggest retrobulbar or intracranial processes, or when sudden visual change is accompanied by headache, neurological signs, or atypical fundus findings.
How are neurology and diagnostics integrated?
Neurology-focused diagnostics address vision loss that arises from the visual pathways or systemic neurological disease. Visual field testing, pattern electroretinography, and visual evoked potentials help localize dysfunction between retina, optic nerve, and cortex. Blood tests and systemic screening may identify inflammatory, infectious, or metabolic contributors. Coordination with neurology is critical when visual symptoms are accompanied by diplopia, pupil abnormalities, weakness, numbness, or cognitive changes; these raise concern for conditions that require urgent investigation.
What role do rehab, glare management, and lighting play?
When diagnostic workups identify treatable causes, targeted therapies follow. Refractive correction, cataract surgery, or retinal interventions address many structural issues. For persistent deficits, visual rehabilitation can improve function: orientation and mobility training, low-vision aids, prism correction, and eccentric viewing techniques. Environmental modifications—reducing glare with polarized lenses, optimizing indoor lighting, and adjusting contrast in living spaces—often yield measurable improvements in daily activities. Early referral to rehab services helps patients adapt while diagnostic and therapeutic plans continue.
Conclusion
A stepwise, multidisciplinary evaluation best addresses unexplained visual changes. Screening and acuity measurements, careful refraction and optics assessment, ocular and retinal imaging, and neurology-linked diagnostics together clarify causes and guide treatment. Incorporating rehabilitative strategies and environmental adjustments helps patients maintain function while definitive care proceeds. Timely, coordinated assessment increases the likelihood of identifying reversible conditions and optimizing visual outcomes.