Respiratory Health and Blood Clot Awareness
Understanding pulmonary embolism is crucial for maintaining respiratory health and recognizing the potential dangers of blood clots. This serious condition occurs when a blood clot, often originating in the deep veins of the legs, travels to the lungs, blocking blood flow. Awareness of its symptoms, risk factors, and preventative measures can significantly impact early detection and effective management, safeguarding overall well-being and reducing severe health complications.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What are the symptoms of a pulmonary embolism?
A pulmonary embolism can manifest with a variety of symptoms, though their severity can depend on the size of the clot and the individual’s overall health. Common indicators often include sudden shortness of breath, which may worsen with exertion, and chest pain that can feel sharp or stabbing, often exacerbated by deep breathing or coughing. Individuals might also experience a cough, sometimes producing blood-tinged sputum, rapid or irregular heartbeat, and lightheadedness or dizziness. In some cases, fainting can occur. Recognizing these symptoms promptly is vital for seeking immediate medical attention, as early awareness and intervention can prevent serious health outcomes.
Understanding the risks and causes of blood clots
Several factors can increase an individual’s risk of developing blood clots, specifically deep vein thrombosis (DVT), which is a primary cause of pulmonary embolism. Prolonged periods of inactivity, such as long flights or bed rest after surgery, can slow blood flow, leading to clot formation. Certain medical conditions like cancer, heart disease, and inherited blood clotting disorders also elevate risk. Surgical procedures, particularly orthopedic surgeries involving the hips or knees, as well as trauma, can increase the likelihood of thrombosis. Hormonal factors, including oral contraceptive use and hormone replacement therapy, and pregnancy, can also contribute to a heightened risk of clot development. Age, obesity, and smoking are additional factors that impact vascular health and can contribute to the formation of dangerous clots.
How is a pulmonary embolism diagnosed?
Diagnosing a pulmonary embolism typically involves a combination of medical history review, physical examination, and specific diagnostic tests. Initial assessments may include blood tests, such as a D-dimer test, which measures a substance released when blood clots break down; however, a positive result requires further investigation. Imaging tests are crucial for confirmation. A computed tomography pulmonary angiography (CTPA) is often the preferred method, using a contrast dye to visualize the pulmonary arteries for blockages. Other tests might include a ventilation-perfusion (V/Q) scan, which assesses air and blood flow in the lungs, or an ultrasound of the legs to check for DVT. Electrocardiograms (ECGs) and chest X-rays can help rule out other conditions with similar symptoms but are not definitive for pulmonary embolism diagnosis.
Approaches to treatment and prevention
Treatment for a pulmonary embolism typically focuses on preventing the clot from growing, stopping new clots from forming, and breaking down existing clots. Anticoagulant medications, often called blood thinners, are the cornerstone of treatment, helping to prevent further clotting. In severe cases, thrombolytic drugs may be administered to dissolve the clot rapidly, though these carry a higher risk of bleeding. For individuals who cannot take anticoagulants, a vena cava filter might be placed in the main vein leading to the lungs to catch clots before they reach the pulmonary arteries. Prevention strategies often mirror risk factor management, including regular movement during long periods of sitting, wearing compression stockings, and taking prescribed anticoagulants if at high risk. Maintaining a healthy lifestyle, avoiding smoking, and managing underlying conditions also contribute significantly to prevention.
The path to recovery and long-term respiratory health
Recovery from a pulmonary embolism can vary depending on the clot’s size, the extent of lung damage, and the individual’s overall health. After initial treatment, ongoing management often involves continued use of anticoagulant medication for several months or longer to prevent recurrence. Regular follow-up appointments with healthcare professionals are essential to monitor progress, adjust medication, and assess long-term respiratory and vascular health. Some individuals may experience persistent shortness of breath or reduced exercise tolerance, which might require pulmonary rehabilitation or other supportive therapies. Adopting a heart-healthy lifestyle, including a balanced diet and regular physical activity, is crucial for supporting recovery and promoting overall well-being. Education about recognizing potential recurrence symptoms is also a key component of long-term care.
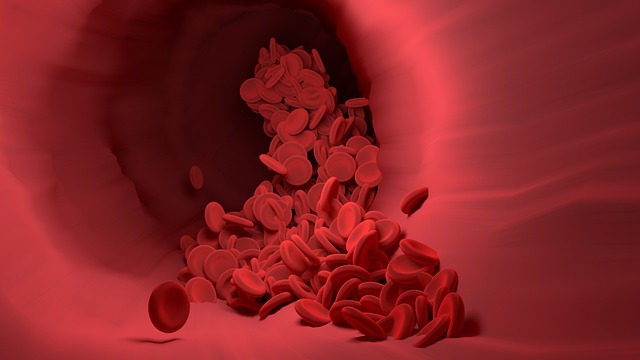
Impact of a blockage on lung and oxygen circulation
A pulmonary embolism directly impacts the lung’s ability to facilitate adequate oxygen circulation throughout the body. When a blood clot causes a blockage in the pulmonary arteries, blood flow to a portion of the lung is restricted. This means that even if air can enter that part of the lung, the oxygen cannot effectively transfer into the bloodstream because there isn’t enough blood reaching the capillaries. Consequently, the body’s tissues and organs may not receive sufficient oxygen, leading to symptoms like shortness of breath and fatigue. A significant blockage can severely strain the heart, as it has to work harder to pump blood through the obstructed pulmonary vasculature, potentially leading to heart failure. The severity of these effects depends on the size and number of clots, highlighting the critical role of unobstructed blood flow for efficient oxygen exchange and overall health.




