Therapeutic Options for Cranial Tumors
Cranial tumors, often referred to as brain tumors, represent a complex group of conditions arising from abnormal cell growth within the brain or its surrounding structures. Understanding the various therapeutic options available is crucial for individuals affected by these diagnoses and their families. This article aims to provide an overview of the current approaches used in managing and treating cranial tumors, highlighting the multidisciplinary effort involved in patient care.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
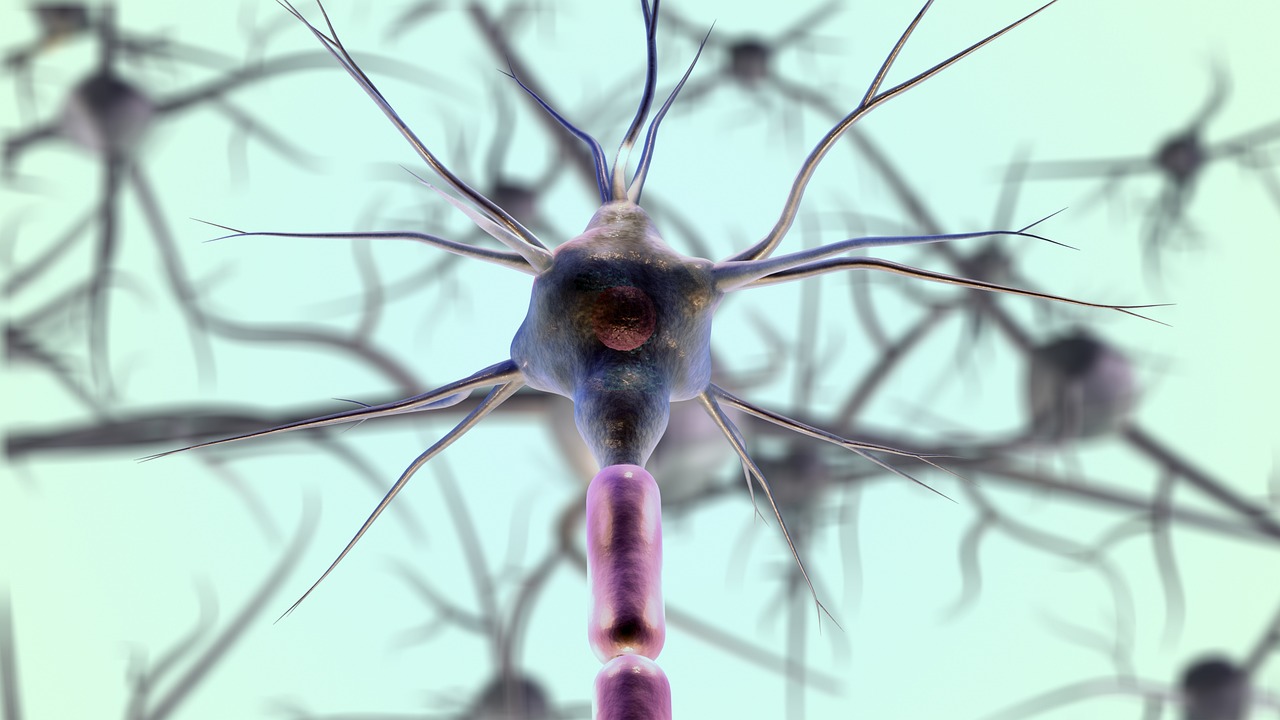
Abnormal cell growth within the brain or its immediate surroundings poses significant challenges due to the vital functions controlled by the nervous system. The identification and characterization of these growths, known as intracranial tumors or lesions, are critical first steps in developing an effective management strategy. Early detection and an accurate diagnosis are paramount for improving outcomes and guiding the subsequent therapeutic journey.
Diagnosis and Detection of Intracranial Tumors
The journey toward managing a cranial tumor typically begins with a thorough diagnosis and detection process. Initial symptoms can vary widely depending on the tumor’s size, location, and rate of growth, often prompting a visit to a neurology specialist. Diagnostic tools are crucial for visualizing these cerebral anomalies. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans are primary imaging techniques used to identify the presence and precise location of a tumor. Further diagnostic clarity often comes from a biopsy, where a small tissue sample is extracted and examined under a microscope by a neuropathologist. This pathological analysis helps in classifying the tumor type, determining its grade, and understanding its unique characteristics, which are all vital for planning appropriate treatment.
Exploring Therapy and Treatment Approaches
Once a diagnosis is established, a range of therapy and treatment options are considered, often involving a team of oncology specialists. The choice of treatment depends on several factors, including the tumor’s type, size, location, the patient’s age, and overall health. Surgical resection is a common approach, aiming to remove as much of the tumor as safely possible while preserving neurological function. Radiation therapy, which uses high-energy rays to destroy cancer cells or shrink tumors, is another cornerstone of treatment. This can include external beam radiation or more targeted approaches like stereotactic radiosurgery. Chemotherapy, utilizing drugs to kill cancer cells, and newer targeted therapies that block specific molecular pathways involved in tumor growth, are also integral components. Immunotherapy, which harnesses the body’s immune system to fight the neoplasm, represents an evolving frontier in treatment strategies.
Advances in Research and Patient Care
The field of neurology and oncology is continuously advancing through dedicated research efforts, leading to more refined treatment options and improved patient care. Ongoing clinical trials explore novel drugs, innovative surgical techniques, and advanced radiation delivery methods. Precision medicine, tailoring treatments based on the genetic makeup of the individual’s tumor, is becoming increasingly prominent. Comprehensive patient care extends beyond initial treatment, encompassing a multidisciplinary team approach involving neurosurgeons, radiation oncologists, medical oncologists, neurologists, and supportive care specialists. This collaborative model ensures that every aspect of the patient’s well-being is addressed throughout their treatment journey.
Rehabilitation and Prognosis After Treatment
Following active treatment, rehabilitation plays a critical role in helping patients regain lost functions and improve their quality of life. Rehabilitation programs can include physical therapy to address motor deficits, occupational therapy to assist with daily living activities, and speech therapy for communication challenges. The extent and type of rehabilitation depend on the specific neurological impact of the tumor and its treatment. Prognosis, which refers to the likely course of a medical condition, varies significantly among individuals and depends heavily on factors such as tumor type, grade, response to treatment, and overall health status. Long-term follow-up and supportive care are essential for monitoring recovery and managing any lingering effects.
Understanding Tumor Growth and Pathology
Cranial tumors can be broadly categorized as primary, originating within the brain, or metastatic, spreading to the brain from another part of the body. They are also classified as benign (non-cancerous) or malignant (cancerous), with malignant tumors typically exhibiting more aggressive growth and a higher potential for spread. The pathology of a tumor, or the study of its disease, provides crucial insights into its cellular structure and behavior. Understanding the specific characteristics of tumor growth, including its size, location, and how it interacts with the surrounding nervous system, is fundamental for clinicians. This detailed pathological understanding guides treatment decisions, helping to determine the most effective approach to manage the lesion and prevent further progression of the neoplasm.
Managing cranial tumors requires a comprehensive and individualized approach, integrating advanced diagnostic techniques with a diverse array of therapeutic options. From initial diagnosis and treatment planning to post-treatment rehabilitation and ongoing patient care, the focus remains on enhancing outcomes and improving the quality of life for those affected. Continued research and collaborative efforts in the medical community are pivotal in advancing our understanding and capacity to address these complex neurological conditions.




