Glaucoma Treatment: Options, Care, and When to See a Specialist
Glaucoma is a group of eye conditions that damage the optic nerve and can cause progressive, irreversible vision loss if untreated. Treatment focuses on lowering intraocular pressure (IOP) and protecting the optic nerve to slow or prevent further loss. This article explains common treatment approaches, the roles of medical professionals, and what to expect from ongoing care so you can discuss options with your eye doctor or specialist.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
How does glaucoma affect the eye?
Glaucoma most often damages the optic nerve by increased pressure inside the eye, though some forms occur with normal pressures. Damage usually progresses slowly and without pain, which is why regular eye exams matter. Structural changes can be detected with optic nerve imaging and visual field testing. Early detection gives more treatment options; late-stage damage cannot be reversed but further loss can often be slowed. Discussing test results with an eye doctor helps clarify the severity and likely treatment pathways based on your specific eye anatomy and optic nerve status.
When should you see an eye doctor?
An eye doctor should be seen for routine screenings—especially if you have risk factors such as family history, high eye pressure, older age, diabetes, or certain ethnic backgrounds. See a doctor promptly if you notice sudden vision changes, severe eye pain, or nausea accompanied by eye redness; those can signal acute angle-closure glaucoma, a medical emergency. For chronic glaucoma, follow-up intervals vary from a few months to a year based on disease stability. Ask your eye doctor about frequency of examinations, imaging tests, and visual field monitoring.
What medical treatments are available?
Medical treatment usually begins with prescription eye drops that reduce eye pressure by decreasing fluid production or improving outflow. Classes include prostaglandin analogs, beta-blockers, carbonic anhydrase inhibitors, alpha agonists, and rho-kinase inhibitors. Oral medications are less commonly used but may be prescribed in some situations. Side effects and interactions should be reviewed with your prescribing physician. Medication adherence is critical — missed doses can allow pressure to rise and increase risk of progression. Your doctor may try different agents to balance effectiveness and tolerability.
When is a glaucoma specialist recommended?
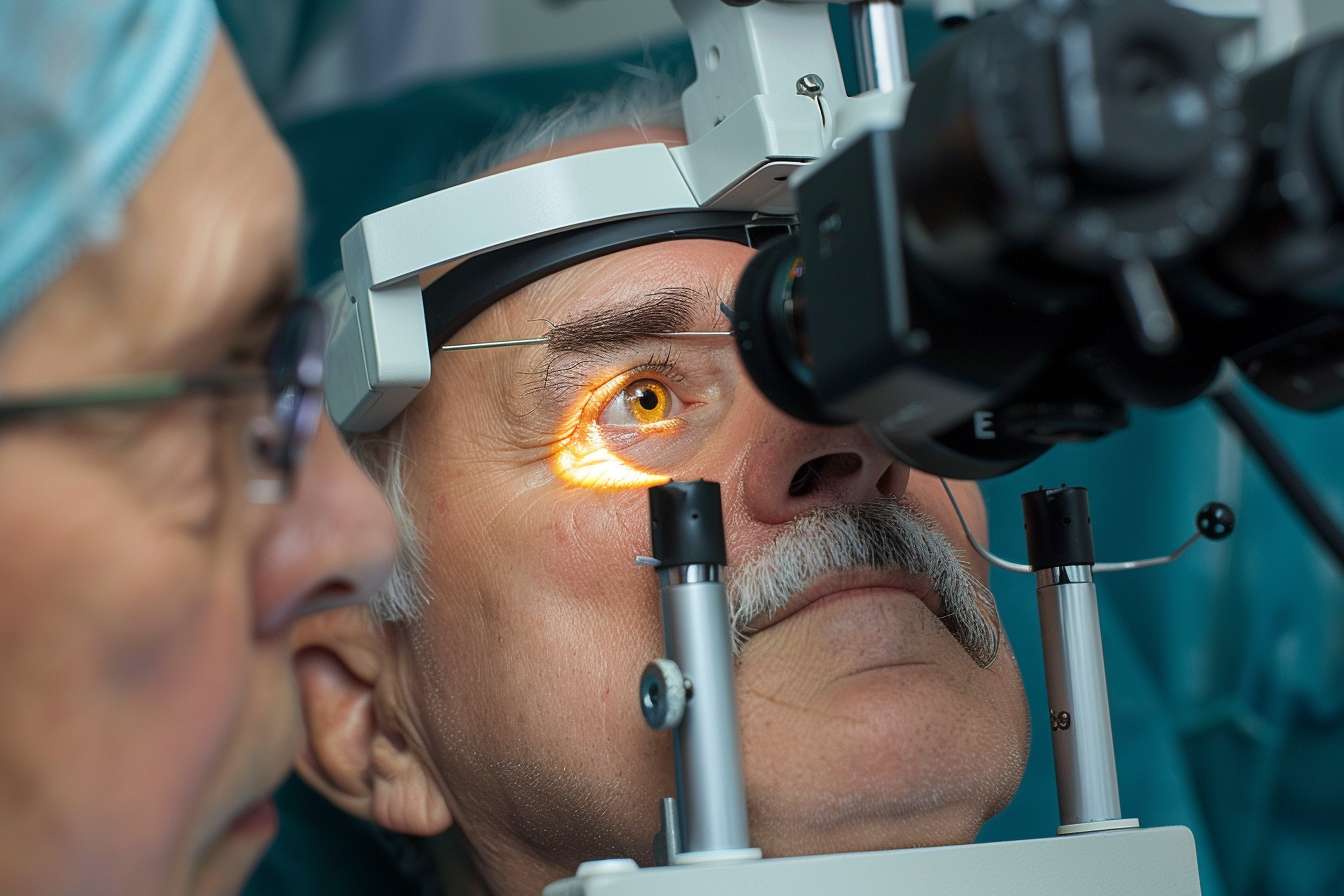
A glaucoma specialist is an ophthalmologist with advanced training in glaucoma management and surgery. Referral to a specialist is appropriate when glaucoma is advanced, progressing despite treatment, when secondary or complicated glaucoma is present, or when surgical intervention is being considered. A specialist can offer advanced imaging interpretation, tailored surgical options, and participation in clinical trials when appropriate. If your general eye doctor recommends a specialist, ask about the reasons for referral and what outcomes and risks to expect from additional procedures or monitoring.
What surgical and laser options exist for glaucoma?
Laser and surgical options are considered when medications and laser therapies are insufficient or not tolerated. Laser procedures include selective laser trabeculoplasty (SLT) to improve drainage and laser peripheral iridotomy for certain angle-closure conditions. Surgical choices range from minimally invasive glaucoma surgeries (MIGS) to trabeculectomy and glaucoma drainage devices (tube shunts). MIGS tend to have quicker recovery and lower complication rates but may provide more modest pressure reduction compared with traditional surgeries. Each option has specific indications, risks, and benefits that your specialist and medical team will review based on your glaucoma type and target eye pressure.
Conclusion
Managing glaucoma is a long-term process that combines regular monitoring, medical therapy, possible laser or surgical intervention, and close communication with your eye doctor or glaucoma specialist. Early detection and adherence to the recommended treatment plan are key to slowing progression and preserving vision. Discuss test results, treatment goals, and follow-up schedules with your medical team to create a care plan suited to your condition and lifestyle.




