Glaucoma Treatment: Options, Care, and Follow-up
Glaucoma is a group of conditions that damage the optic nerve and can lead to irreversible vision loss if untreated. Treatment aims to lower intraocular pressure (IOP) or protect the optic nerve to slow or stop progression. Management often requires ongoing monitoring, medication adherence, and sometimes procedural or surgical intervention tailored to the type and stage of glaucoma and the patient’s overall health.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What is glaucoma?
Glaucoma refers to several eye disorders that share progressive optic nerve damage, often associated with elevated intraocular pressure. Primary open-angle glaucoma is the most common form and progresses slowly, sometimes without symptoms until noticeable vision loss occurs. Other forms include angle-closure glaucoma, normal-tension glaucoma, and secondary glaucomas caused by trauma, inflammation, or other medical conditions. Diagnosis relies on a combination of eye pressure measurement, optic nerve examination, visual field testing, and imaging of the optic nerve and retinal nerve fiber layer. Early detection is important because damage is usually permanent but progression can be slowed.
When to see an eye doctor?
Regular eye examinations are the primary way to detect glaucoma early. Adults over 40, people with a family history of glaucoma, those with high eye pressure, certain ethnic groups, and people with conditions such as diabetes or high myopia should have periodic screening exams by an eye doctor. Symptoms prompting immediate evaluation include sudden vision changes, severe eye pain, nausea with eye pain, or halos around lights — signs that may indicate angle-closure glaucoma, which requires urgent care. Routine visits allow IOP checks, visual field tests, and documentation of optic nerve health to guide treatment decisions.
What medical treatments are used?
Medical management usually begins with topical eye drops that lower intraocular pressure by either reducing aqueous humor production or improving outflow. Common classes include prostaglandin analogs, beta blockers, alpha agonists, carbonic anhydrase inhibitors, and Rho kinase inhibitors. Oral medications are less frequently used but may be prescribed short-term when drops are insufficient or in acute situations. Side effects vary by medication class and can include ocular irritation, changes in eyelash growth or eye color, systemic effects like slowed heart rate or bronchospasm, and dry mouth. Adherence is critical: missed doses can allow pressure to rise and increase risk of progression. Your eye doctor will choose treatments based on glaucoma type, target pressure, comorbidities, and tolerance.
When is a specialist needed?
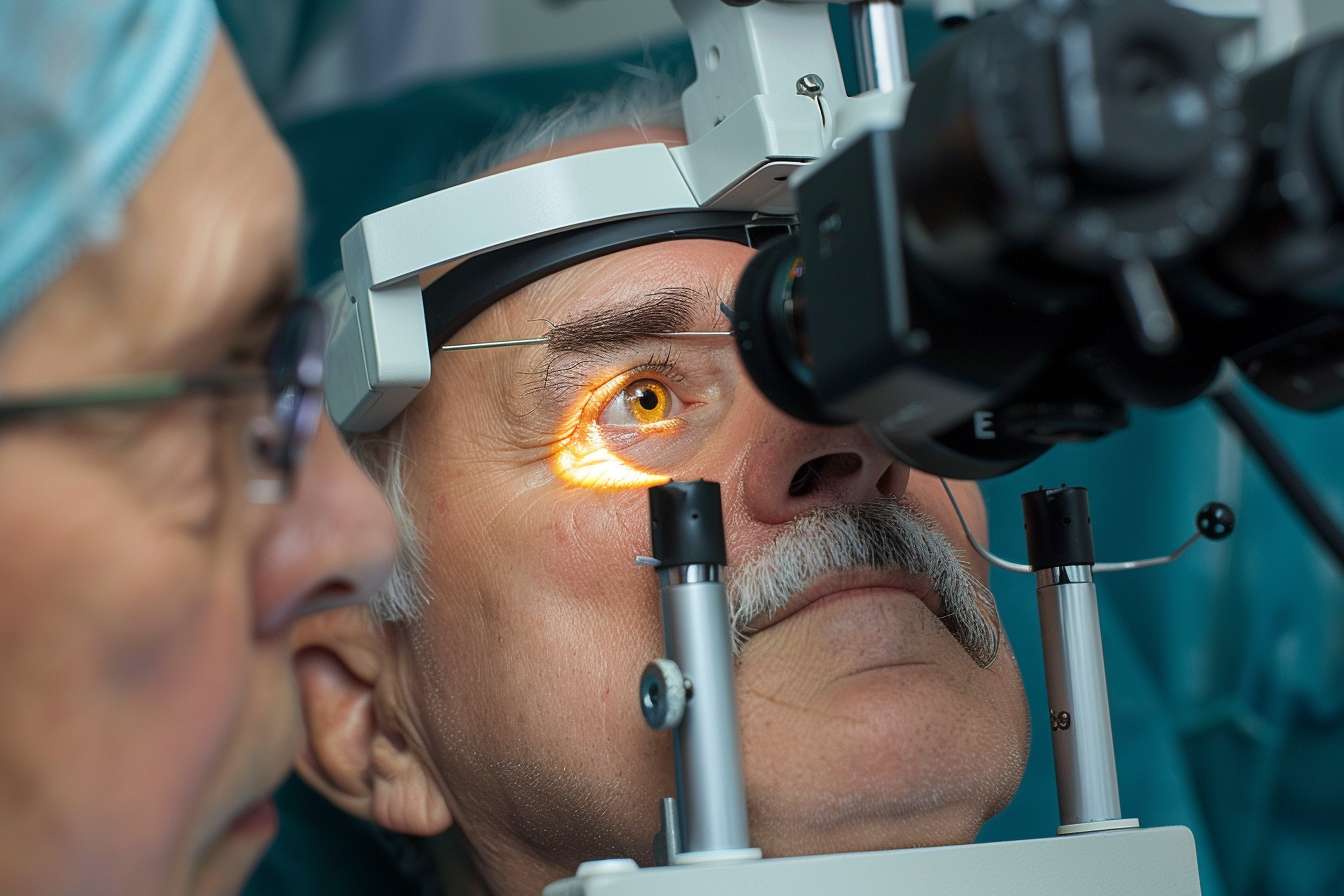
An ophthalmologist who specializes in glaucoma (a glaucoma specialist) is typically involved for progressive disease, complex cases, or when surgical or laser options are considered. General ophthalmologists manage many straightforward cases, but referral to a specialist may be appropriate for rapidly progressing optic nerve damage, very high IOP, coexisting ocular conditions, or when multiple medications fail to control pressure. A glaucoma specialist can perform or recommend advanced diagnostics, tailor a long-term management plan, and offer a wider range of procedural and surgical interventions. Communication between primary eye care providers and specialists helps ensure coordinated follow-up and monitoring.
Surgical and laser glaucoma treatments
When medications do not achieve target IOP, laser or surgical procedures can improve outflow or create alternative drainage pathways. Laser trabeculoplasty, including selective laser trabeculoplasty (SLT), is often used for open-angle glaucoma to enhance drainage and can be an initial therapy or adjunct to drops. For more advanced or refractory cases, surgical options include trabeculectomy, tube shunt implants, and a growing set of minimally invasive glaucoma surgeries (MIGS). Each procedure has distinct risks and potential benefits: trabeculectomy can produce substantial IOP reduction but carries higher complication risk, while MIGS tends to be safer but may reduce pressure less. Choice of procedure depends on disease severity, anatomy, prior surgeries, and patient-specific goals.
Monitoring, lifestyle, and long-term care
Glaucoma management is long-term. Regular follow-up visits track IOP, visual fields, and optic nerve imaging to detect change and adjust treatment. Patients should report any new visual symptoms promptly. Lifestyle measures such as controlling systemic blood pressure, avoiding medications that may increase eye pressure, and protecting the eyes from injury can support overall eye health. Adherence to prescribed therapies and attending scheduled appointments are among the most important factors in preserving vision. For access to care, ask your eye doctor about glaucoma specialists and local services or referral pathways if you require advanced treatment or closer monitoring.
Conclusion
Glaucoma treatment focuses on preserving vision by lowering intraocular pressure and protecting the optic nerve through medications, laser therapy, or surgery, combined with regular monitoring. Decisions about therapy are individualized, balancing expected pressure reduction, side effects, and patient circumstances. Early detection and ongoing follow-up with an eye doctor and, when appropriate, a glaucoma specialist improve the likelihood of maintaining functional vision over time.




