Glaucoma Treatment: Options, Roles, and Ongoing Care
Glaucoma is a group of eye conditions that can damage the optic nerve and lead to vision loss if not managed. Treatment aims to lower eye pressure, preserve vision, and slow progression through medication, procedures, or surgery. Early detection and consistent follow-up are central to better outcomes, since damage is often gradual and irreversible.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What is glaucoma and how does it affect the eye?
Glaucoma commonly causes progressive loss of peripheral vision and, in advanced stages, central vision loss. The most frequent form, open-angle glaucoma, develops slowly and may go unnoticed without screening. Angle-closure glaucoma is less common but can present suddenly with pain and vision changes that require immediate medical attention. Pathways of damage typically involve raised intraocular pressure or impaired blood flow to the optic nerve, but the condition varies by individual and subtype.
Many people with glaucoma have no symptoms in early stages, which is why routine eye examinations and pressure checks are recommended, especially for those with risk factors such as age, family history, or certain medical conditions.
When should you see an eye doctor for glaucoma?
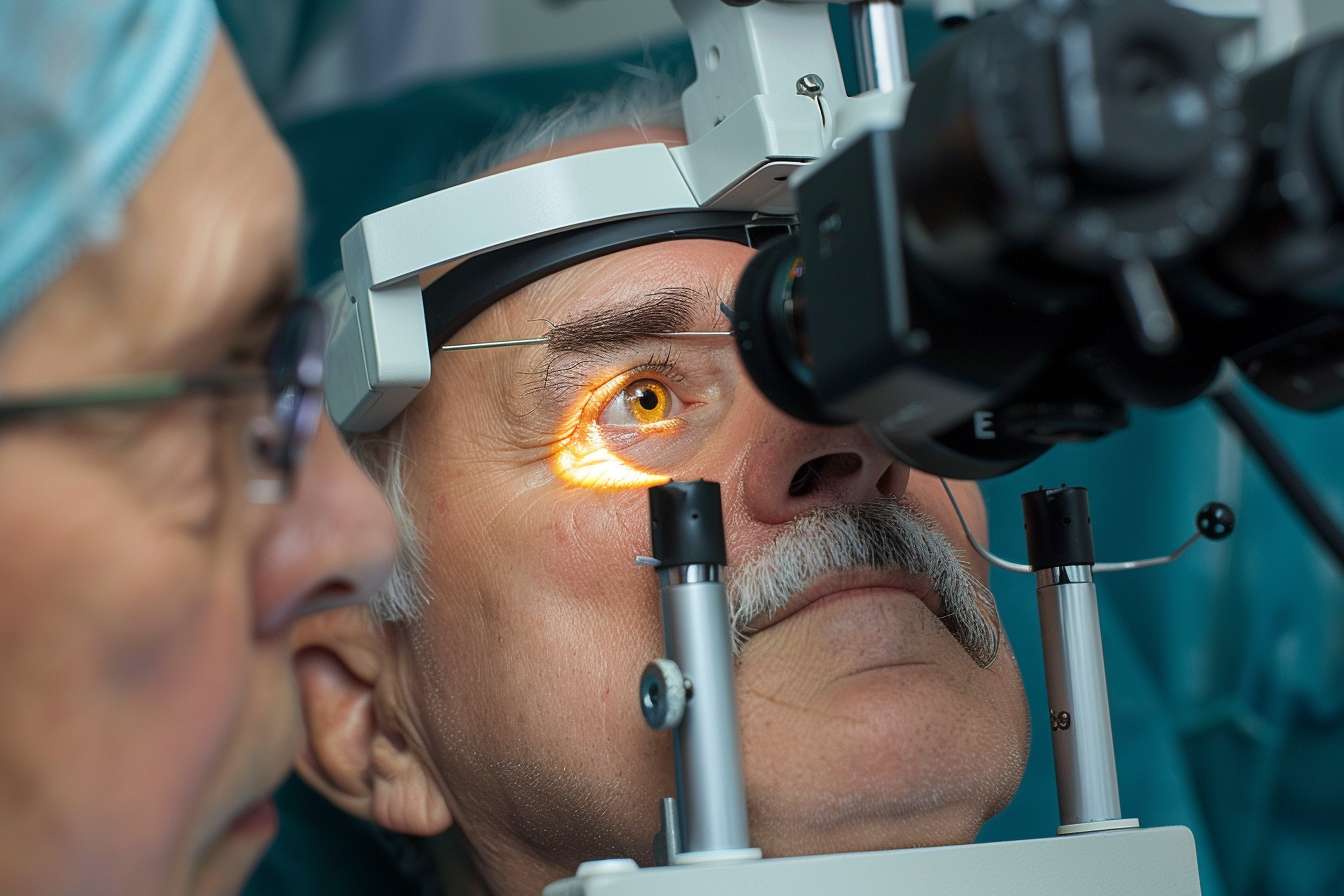
An eye doctor (optometrist or ophthalmologist) should evaluate anyone with risk factors, visual changes, or a family history of glaucoma. Routine comprehensive eye exams include measurements of intraocular pressure, optic nerve assessment, and visual field testing to detect early changes. If screening tests suggest glaucoma, referral to an ophthalmologist for further evaluation often follows.
If you experience sudden eye pain, severe headache, nausea with blurred vision, or rapid vision loss, seek immediate medical attention, as these can be signs of acute angle-closure glaucoma.
What medical treatments are available for glaucoma?
Initial medical treatment typically uses topical eye drops to lower intraocular pressure by reducing fluid production or increasing drainage. Common classes include prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors. Systemic medications may be used short-term in acute situations.
Medication adherence, correct drop technique, and monitoring for side effects or interactions with other medical treatments are important. If drops are insufficient or not tolerated, laser or surgical options may be discussed with your treating doctor.
When is a specialist needed for glaucoma care?
A glaucoma specialist—an ophthalmologist with advanced training—becomes important for progressive or complex cases, uncontrolled pressure despite treatment, or when surgical or laser intervention is considered. Specialists can assess optic nerve damage, interpret advanced imaging, and recommend procedures such as selective laser trabeculoplasty, minimally invasive glaucoma surgeries (MIGS), trabeculectomy, or tube shunt implantation depending on disease severity and patient factors.
Coordinated care with other medical specialists may be required when systemic conditions or medications influence eye health. Decisions about surgery should weigh potential benefits, risks, and the patient’s overall health and lifestyle.
What follow-up, monitoring, and local services support glaucoma care?
Glaucoma requires ongoing monitoring to track pressure, optic nerve status, and visual fields. Typical follow-up schedules vary with severity—from every few months for active disease to annual checks for stable, early-stage disease. Local services often include primary eye care from optometrists, ophthalmology clinics, and hospital-based glaucoma units; access to visual field testing and optical coherence tomography (OCT) imaging is valuable.
When arranging care in your area, consider whether the provider offers comprehensive testing, communication with your medical team, and access to treatment options. Patient education, low-vision support services, and resources for medication assistance can also be part of local services.
Conclusion
Glaucoma treatment is tailored to the individual and focuses on preventing further optic nerve damage through pressure-lowering strategies, monitoring, and timely interventions. Regular exams with an eye doctor and, when needed, referral to a glaucoma specialist improve the chances of preserving vision. Because glaucoma can be asymptomatic early on, adherence to follow-up and treatment plans is a cornerstone of long-term eye health.





