Minimizing Scarring: Aftercare Practices Following Minor Skin Lesion Treatments
Effective aftercare after minor skin lesion treatments helps support healing and can reduce visible scarring and pigmentation changes. This overview highlights practical, evidence-informed steps to follow after outpatient procedures such as excision, biopsy, or laser treatment, and explains when to contact a clinic or specialist.
This article outlines practical aftercare practices following minor skin lesion treatments, focusing on approaches that support healing and reduce scarring and pigmentation changes. It covers common outpatient procedures, wound care basics, clinic follow-up and signs that warrant a consultation. This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
What to expect after a dermatology procedure
Minor dermatology procedures—such as excision, shave removal, biopsy, or laser therapy—typically produce a small wound that begins the natural healing cascade immediately. Early stages may include redness, mild swelling, and a scab or crust as the skin repairs. Understanding normal symptoms helps separate routine healing from complications. Most benign lesions heal uneventfully in days to weeks in an outpatient setting, but individual factors such as skin type, lesion location, and previous scarring tendency influence outcomes.
Managing wounds after excision or biopsy
Proper wound care after an excision or biopsy directly affects scarring. Keep the area clean and follow the clinic’s instructions about cleansing frequency and products. Gentle soap and water are usually sufficient; avoid harsh scrubs. Protect sutured wounds according to timing advised by your clinician—typically sutures on the face are removed sooner than on the body. Apply recommended ointments or dressings to maintain a moist healing environment, which can reduce scar prominence. Avoid picking at scabs or removing sutures early, as doing so increases the risk of wider scars and pigmentation changes.
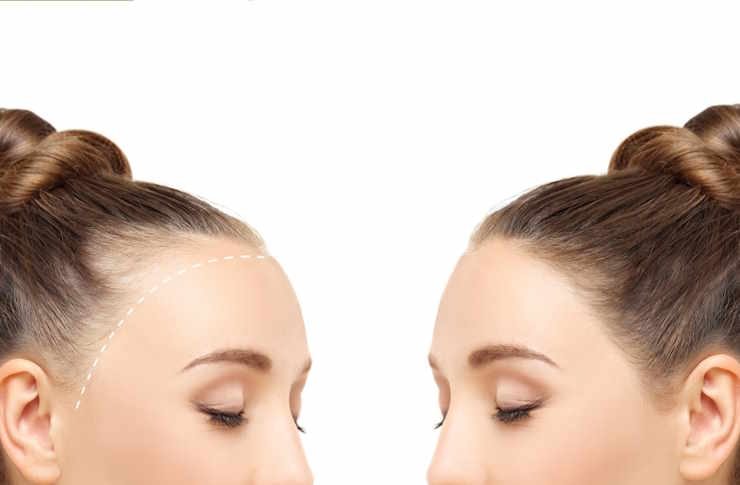
Caring for pigmentation and scarring after laser or removal
Pigmentation shifts—lighter or darker patches—can follow trauma to the skin, including laser or excision. Sun protection is essential because ultraviolet exposure increases the risk of persistent hyperpigmentation. Use a broad-spectrum sunscreen and consider physical barriers like hats when outdoors. For scars, silicone gel sheets or topical silicone formulations are commonly advised to flatten and soften raised scars after the wound is closed. Discuss options such as topical retinoids or professional treatments with a dermatologist if pigmentation or keloid tendencies are a concern.
Clinic follow-up, consultation, and outpatient guidance
Attend scheduled follow-up appointments so your clinician can assess healing, remove sutures if needed, and confirm histology results if a biopsy was done. A timely consultation is important if pathology reveals unexpected findings or if the lesion is not clearly benign. Clinics providing outpatient dermatology care can also advise on scar-minimizing strategies tailored to your skin type and the procedure performed. Keep records of any instructions given at the clinic and ask for clarification about activity restrictions, skincare products, and signs that require prompt review.
When to seek help: infection, delayed healing, or abnormal scarring
Contact your clinic or seek a consultation if you notice increasing pain, spreading redness, pus, fever, or wound separation, as these may indicate infection. Delayed healing beyond the expected timeframe warrants review—especially in patients with underlying conditions such as diabetes. If raised, firm, or rapidly enlarging scars develop (hypertrophic scars or keloids), early discussion about management options can improve results. A dermatologist can recommend treatments including steroid injections, silicone therapy, or referral for procedural revision when appropriate.
Practical aftercare tips to support healing and reduce scarring
Simple, consistent steps support optimal outcomes: follow cleansing and dressing instructions from your clinic; avoid smoking, which impairs healing; protect the area from sun exposure to limit pigmentation; maintain a balanced diet and hydration to support tissue repair. For wounds that closed by secondary intention (left to heal without sutures), patience and gentle care are important. If laser therapy or excision was used, ask about the timing for introducing topical scar therapies. Document any changes and keep a consultation scheduled if you have concerns about benign versus suspicious features of a lesion.
Conclusion
Minimizing scarring after minor skin lesion procedures involves a combination of accurate information from your clinic, consistent wound care, sun protection, and timely follow-up. Individual healing varies, and consultation with a dermatologist or qualified clinician helps tailor aftercare—particularly when pigmentation changes or abnormal scarring arise. This article provides general guidance but does not replace personalized medical advice.




