The Role of Blood Clots in Respiratory Function
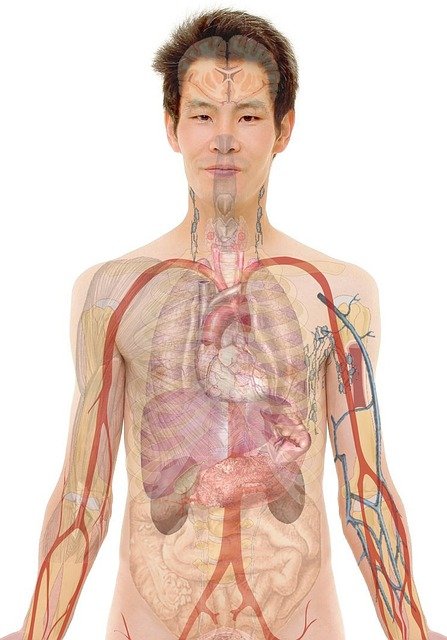
Pulmonary embolism, a serious medical condition, occurs when a blood clot travels to the lungs, obstructing the pulmonary arteries. This blockage can significantly impair the body's ability to exchange oxygen and carbon dioxide, leading to potentially life-threatening consequences. Understanding the mechanisms behind this condition, from the formation of the initial clot to its impact on respiratory health, is crucial for both prevention and timely intervention.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Pulmonary embolism represents a critical health concern characterized by the presence of a blood clot, or embolus, within the arteries of the lungs. These clots typically originate in other parts of the body, most commonly the deep veins of the legs, a condition known as deep vein thrombosis (DVT). Once dislodged, the clot travels through the bloodstream to the heart and then into the pulmonary circulation, where it can become lodged in a pulmonary artery. This obstruction disrupts the normal flow of blood to parts of the lungs, severely affecting their capacity to oxygenate blood and remove carbon dioxide.
How Do Blood Clots Impact Lung Vascular Function?
When a blood clot obstructs a pulmonary artery, it creates a physical blockage that prevents blood from reaching the lung tissue responsible for gas exchange. This interruption in the vascular supply means that even if air enters the alveoli (tiny air sacs in the lungs), the blood flowing past them cannot pick up oxygen or release carbon dioxide. The severity of this impact depends on the size of the clot and the number of arteries affected. A large clot can cause a significant decrease in the body’s oxygen levels and place immense strain on the heart, which must work harder to pump blood through the narrowed or blocked vessels.
Understanding Deep Vein Thrombosis and Pulmonary Circulation
Deep vein thrombosis (DVT) is the primary source of the clots that lead to pulmonary embolism. DVT involves the formation of a blood clot in a deep vein, usually in the leg or pelvis. Factors contributing to thrombosis include prolonged immobility, surgery, certain medical conditions, and genetic predispositions. Once a DVT forms, there is a risk that a piece of the clot can break off, becoming an embolus. This embolus then travels through the venous system, passes through the right side of the heart, and enters the pulmonary artery, initiating a pulmonary embolism and disrupting normal circulation to the lungs.
Recognizing Symptoms and the Need for Prompt Diagnosis
The symptoms of a pulmonary embolism can vary widely but often include sudden shortness of breathing, chest pain that worsens with deep breaths, coughing (sometimes with blood), and a rapid heart rate. Other signs might include lightheadedness or dizziness. Because these symptoms can mimic other conditions, an accurate and prompt diagnosis is crucial. Diagnostic methods often include a physical examination, blood tests (such as D-dimer), imaging tests like CT pulmonary angiography, ventilation-perfusion scans, and ultrasound of the legs to check for DVT. Early identification of the blockage is key to preventing severe complications and ensuring effective treatment.
Strategies for Prevention and Effective Treatment Approaches
Prevention of pulmonary embolism largely focuses on mitigating the risk factors for DVT. This includes maintaining an active lifestyle, avoiding prolonged periods of immobility, especially during long travel, and using compression stockings or anticoagulant medications for individuals at high risk. For those who have developed a DVT or pulmonary embolism, treatment typically involves anticoagulant medications to prevent the clot from growing and to stop new clots from forming. In some severe cases, thrombolytic drugs may be used to dissolve existing clots, or surgical interventions like embolectomy might be necessary to remove the blockage. Long-term management often involves continued anticoagulation and lifestyle adjustments to improve overall health.
Understanding the intricate relationship between blood clots and respiratory function underscores the importance of recognizing the signs of deep vein thrombosis and pulmonary embolism. The body’s ability to absorb oxygen and expel carbon dioxide is fundamental to life, and any compromise to this system, particularly due to a vascular blockage, demands immediate attention. Ongoing research continues to refine both preventive strategies and treatment protocols, aiming to improve outcomes for individuals affected by this serious condition and safeguard their breathing health.